Summary
Standardized, comprehensive and fully quantitative testing of autonomic functions is described. The autonomic tests consist of evaluation of all three major autonomic domains including cardiovagal, adrenergic and sudomotor. The severity and distribution of dysautonomia is quantitated using Composite Autonomic Severity Scores.
Abstract
Disorders associated with dysfunction of autonomic nervous system are quite common yet frequently unrecognized. Quantitative autonomic testing can be invaluable tool for evaluation of these disorders, both in clinic and research. There are number of autonomic tests, however, only few were validated clinically or are quantitative. Here, fully quantitative and clinically validated protocol for testing of autonomic functions is presented. As a bare minimum the clinical autonomic laboratory should have a tilt table, ECG monitor, continuous noninvasive blood pressure monitor, respiratory monitor and a mean for evaluation of sudomotor domain. The software for recording and evaluation of autonomic tests is critical for correct evaluation of data. The presented protocol evaluates 3 major autonomic domains: cardiovagal, adrenergic and sudomotor. The tests include deep breathing, Valsalva maneuver, head-up tilt, and quantitative sudomotor axon test (QSART). The severity and distribution of dysautonomia is quantitated using Composite Autonomic Severity Scores (CASS). Detailed protocol is provided highlighting essential aspects of testing with emphasis on proper data acquisition, obtaining the relevant parameters and unbiased evaluation of autonomic signals. The normative data and CASS algorithm for interpretation of results are provided as well.
Protocol
1. Equipment, data acquisition and processing of autonomic signals
As a bare minimum, the clinical autonomic laboratory has to have motorized tilt table, ECG, noninvasive beat-to-beat blood pressure monitor, respiratory monitor and a mean to evaluate sudomotor functions. Recommended equipment is listed at Table 9. The data acquisition and analyzing software is a critical to be able to run the lab effectively. Unfortunately, the commercially suitable software has some restrictions and most of the autonomic laboratories wrote their own acquisition or analyzing software in house. Robust R wave detection and detection of corresponding systolic/diastolic values in blood pressure, eventually in blood flow, is of paramount importance. At University of Massachusetts we use ADInstrument-based recording system (Figures 1-4, Table 9) that is easy to program and provides many mathematical functions in real time.
The protocol use in the paper is based on methodology developed primary by Dr. P. Low and his team (1). This paper assumes that the reader knows how to correctly place ECG electrodes, setup of the continuous blood pressure monitor and how to record the data. Details of the electrode/sensor placement and recommended standards for data acquisition are at reference 4.
2. Deep breathing
Deep breathing tests cardiac parasympathetic functions. Because the heart responses to deep breathing are mediated by the vagal nerve, the test is also referred to as cardiovagal testing. Deep breathing evaluates changes in the instant heart rate that is provoked by “deep” breathing at 6 breaths/min. The test is performed in supine position. The test starts with a rest period that gives patient time to relax. We usually record one minute baseline before proceeding with the deep breathing test.
- Obtain the baseline for one minute, instruct subject to relax.
- Instruct subject to inhale for 5 seconds and exhale for 5 seconds. This 10 second respiratory cycle should be repeated 6 times. Patient should breathe continuously and regularly. Respirator movement should resemble a wave. Sudden inhalations/exhalations or holding the breath should be avoided. Care should be taken not to hyperventilate. Preferentially, breathing should be done through nostrils with closed mouth and the end tidal CO2 should be monitored to rule out hyperventilation
- Calculate the respiratory sinus arrhythmia (RSA). RSA amplitude is defined as the difference between the end of expiration and end of inspiration in heart rate. Typically, 6 respiratory cycles are identified (Figure. 5) and the respective RSA amplitudes are averaged.
Normative values
Normative data are at Table 1.
Interpretation of results
Deep breathing test measures cardiovagal functions. Both deep breathing and Valsalva maneuver are needed for grading of cardiovagal functions. Valsalva maneuver and grading of cardiovagal impairment is described below.
3. Valsalva maneuver
Valsalva maneuver evaluates: 1) sympathetic adrenergic functions using the blood pressure responses ; and 2) cardiovagal (parasympathetic) functions using the heart rate responses. Valsalva maneuver consists of forced expiration against the resistance with the expiratory pressure during strain at 40 mm Hg for 15 seconds.
Mouthpiece assembly
The easy way to measure the expiratory pressure is to connect the pressure gauge to the 5-10 ml plastic syringe and to blow inside the syringe or any similar mouthpiece. There should be a small air leak in the tubing to prevent closing of the glottis.
Technique
Valsalva maneuver is usually performed in supine position. If Valsalva maneuver shows a square-box response and no heart failure is suspected, the table can be turned up 30 degree that can change the Valsalva maneuever to more common four phase pattern.
- Let the subject practice at least one Valsalva maneuver for short time (seconds) until the subject is comfortable with the procedure.
- Wait approximately 1 minute to allow the subject to be relaxed.
- Instruct the subject to: “Take deep breath and blow into the syringe. Keep the pressure 40 mm Hg for 15 seconds”. The subject should see the expiratory pressure as he can adjust the strain. Give the subject feedback how many seconds left. If the pressure is suboptimal, instruct subject to correct the pressure or repeat the Valsalva maneuver.
- Wait 3 minutes.
- Repeat Valsalva maneuver twice, total 3 times
- Select the most representative maneuver for evaluation.
- Obtain the following parameters from Valsalva maneuver (Figure 9 and Figure 11):
- Valsalva ratio.
- Maximal drop of the mean blood pressure during phase 2.
- The peak of the mean blood pressure at the end of late phase 2 (recovery).
- Overshoot, phase 4.
- Maximal pulse pressure drop during phase 2
- Pressure recovery time
Normative values:
Normative values are at Table 2 and Table 3.
Interpretation of results
Valsalva maneuver evaluates both adrenergic and cardiovagal functions. Grading of adrenergic impairment requires both Valsalva maneuver and tilt test. Grading of cardiovagal impairment requires both deep breathing and Valsalva ratio.
4. Tilt testing
The test stimulates the autonomic nervous system with orthostatic stress by passive movement from a supine position to an upright tilt in a controlled laboratory setting.
Technique
- Ensure proper placement of the blood pressure sensor. Ideal blood pressure has well defined dicrotic notch and there is no drift of the baseline.
- Get the baseline blood pressure from the brachial artery.
- Acquire the 5-10 minutes baseline
- Tilt patient up. The tilt should be done at 70 degree. The transition from supine to tilt position should smooth and of duration 5-10 seconds.
- Obtain the blood pressure from a brachial artery every minute.
- Observe subject for the presence of any discomfort, chest pain, shortness of breath, dizziness, lightheadedness, syncope. Be prepared to terminate the tilt of any serious event occurs during the tilt based on clinical judgment.
- Typical duration of the tilt should be 10 minutes. The tilt can be continued if no obvious abnormalities are detected but a clinical history is strongly suggestive of dysautonomia or blood pressure instability.
- Tilt the patient back.
Normative values:
The normal responses in heart rate during the tilt is heart rate increment within 10 – 30 beats per minute. At the same time the maximal heart rate should be less than 120 beats per minute. Normal responses in the blood pressure during the tilt is drop of the systolic blood pressure less than 30 mm Hg or drop of the mean blood pressure less than 20 mm Hg.
Interpretation of results
Tilt tests predominantly evaluates adrenergic functions. Grading of adrenergic impairment requires results from both Valsalva maneuver and tilt test and is described in section 6.
5. Sudomotor testing (QSART)
Quantitative Sudomotor Axon Reflex Test (QSART) evaluates the postganglionic sympathetic cholinergic functions. Most commonly used devices is the Q-Sweat made by WR Medical Electronic. There are 2 types of responses: spontaneous and evoked. Typically larger capsules (sampling area 5.06 cm2, volume 3.614 cm3 ) are used for spontaneous responses and smaller capsules (sampling area 0.7871 cm2, volume 0.1229 cm3) for evoked responses. In the following, all applies for the smaller capsule. For the stimulation, typical settings are: current 2 mA, 5 minutes,
- Assemble the capsules according to the manufacturer recommendation (Figure 20).
- Clean the recording sites vigorously with the alcohol. Recording sites are:1) the medial forearm (75 % distance from the ulnar epicondile to the pisiform bone); 2) the proximal leg (5 cm distal to the fibular head laterally); 3) the distal leg (5 cm proximal to the medial malleolus medially); 4) proximal foot over the extensor digitorum brevis muscle.
- Place the capsules water-tight (Figure 21).
- Fill the capsules with 10% acetylcholine diluted in sterile water (not normal saline !).
- Start sweat recording and verify on the Q-Sweat machine that no leak is present. In the case of the leak, fix the capsule placement.
- Place the ground for stimulation about 5 cm next to the capsule.
- Wait until the baseline sweat is flat, below 100 nanoliters/minute and all channels give similar baseline sweat output (difference < 15 %, Figure 22-23).
- Start stimulation at current 2 mA for 5 minutes, turn on the marker (Figure 24).
- Record another 5 minute of the sweat (total 10 minutes), turn on the marker.
- Obtain the latencies and volumes at each site (Figure. 25)
Normative values
Normative values are at Table 4.
Interpretation of results
Grading of sudomotor impairment is below
6. Grading of autonomic impairment using the Composite Autonomic Severity Score (CASS)
CASS score provides unbiased and full quantification of the autonomic functions in cardiovagal, adrenergic and sudomotor domain. Total score has a direct clinical meaning since it ranks the generalized dysautonomia as mild, moderate and severe. I removed some of ambiguities in the original definition of CASS( 3).
The CASS has the following subscores: 1) Cardiovagal (Table 5 ).; 2) Adrenergic (Table 6); and 3) Sudomotor (Table 7).
For calculation of cardiovagal score both deep breathing and Valsalva ratio are required. Adrenergic score requires both Valsalva maneuver and tilt test results. Sudomotor score can be calculated from QSART results or from the thermoregulator sweat test (TST, not described at this paper).
Since the autonomic testing evaluates global autonomic functions, the results are interpreted in term of generalized autonomic failure (GAF). Results are referred to as normal (CASS total score = 0) or abnormal. The abnormalities ranges from mild GAF (total CASS score 1-3), to moderate (total CASS score 4-6), or severe (total CASS score 7-10).
Mild GAF with score 1 is usually of unclear or limited clinical significance. The score higher than 1 is usually clinically significant and usually indicate the presence of autonomic neuropathy.
7. Representative results:
Examples of data acquisitions are at Figure 1-4. All recorded signal should be clearly visible from a distance to a technician enabling the correct any recordings problems immediately. Both raw data and corresponding systolic/diastolic/mean values should be available in real time (Figure 1). The data acquisition system should provide a great amount of flexibility in the setting of the screen, for example it should be easy to change the time scale (Figure 2) or to choose between raw data tracings or numerical values (Figure 3).
Examples of normal and abnormal deep breathing test are at Figure 6-8. For clarity, the length of the bold line in the middle of the y axis correspond to 10 BPM. Normal deep breathing test is at Figure 6. Note that normative data for the deep breathing test are age but not gender dependent (Table 1). Figure 7 shows moderate abnormality of the cardiovagal functions while Figure 8 shows essentially fixed heart rate that is consistent with severe cardiovagal failure.
Figure 9 shows typical 4 phases in Valsalva maneuver. Note that pressure recovery time is calculated from the systolic blood pressure. A square-wave variant of Valsalva maneuver is at Figure 10. Valsalva ratio calculation is shown at Figure 11. Figure 12 shows normal blood pressure responses. Mild (Figure 13), moderate (Figure 14) and severe (Figure 15) adrenergic impairment results in a distinct blood pressure changes provoked by VM.
Figure 16 shows normal responses in heart rate and blood pressure during 10 minutes of tilt test. Mild orthostatic hypotension associated with mild adrenergic impairment is seen at Figure 17 .Note also prominent fluctuations in both blood pressure and blood flow velocity in the middle cerebral artery that can be associated with adrenergic impairment. Severe adrenergic impairment can results in a progressive fall of the blood pressure as is seen in Figure 18. Example of mixed syncope that has features of both vasodepressors and vasovagal responses is at Figure 19.
Normal QSART responses are at Figure 26. Abnormalities ranging from mild to severe sudomotor impairment are at Figures 28-31.
| Age range (years) | Minimum for normal RSA (beats/min) |
| 10-29 | ≥14 |
| 30-39 | ≥12 |
| 40-49 | ≥10 |
| 50-59 | ≥9 |
| 60-69 | ≥7 |
Table 1. Normative values for deep breathing test.
| Variable | Normal value |
| Maximal drop of the MBP during the early phase 2 | ≥ 20 mmHg |
| MBP at late phase 2 (recovery) | ≥ baseline (mm Hg) |
| MBP at phase 4 (overshoot) | > baseline (mm Hg) |
| Maximal pulse pressure drop | ≥ 50% of baseline |
| Systolic pressure recovery time | < 4 seconds |
Table 2. Normative values for Valsalva maneuver in blood pressure.
| Age range (years) | Minimum for normal VR | |
| Women | Men | |
| 10-29 | 1.46 | 1.59 |
| 30-39 | 1.5 | 1.52 |
| 40-49 | 1.51 | 1.44 |
| 50-59 | 1.47 | 1.36 |
| 60-69 | 1.39 | 1.29 |
Table 3. Normative values for Valsalva ratio.
| Male | Age range (years) | ||
| Location | 10 – 29 | 30-49 | ≥ 50 |
| Forearm | 0.38-2.53 | 0.38-2.53 | 0.38-2.53 |
| Proximal leg | 0.80-2.86 | 0.58-2.64 | 0.36-2.42 |
| Distal leg | 0.72-2.79 | 0.52-2.41 | 0.31-2.02 |
| Foot | 0.39-2.02 | 0.35-1.83 | 0.31-1.64 |
| Female | Age range (years) | ||
| Location | 10 – 29 | 30-49 | ≥ 50 |
| Forearm | 0.10-1.39 | 0.10-1.39 | 0.10-1.39 |
| Proximal leg | 0.23-1.99 | 0.23-1.99 | 0.23-1.99 |
| Distal leg | 0.32-1.51 | 0.21-1.21 | 0.10-0.90 |
| Foot | 0.10-1.38 | 0.08-1.28 | 0.05-1.19 |
Table 4. Normative values for Q-Sweat machine. All values are in microliters.
| Resultados | Degree of abnormality | Cardiovagal score | |
| Value | Definition | ||
| Normal | 0 | ||
| Abnormal | Mild | 1 | Deep breathing or Valsalva ratio reduced but ≥* 50% of minimal normal value |
| Moderate | 2 | Deep breathing or Valsalva ratio reduced to < 50% of minimal normal value | |
| Severe | 3 | Both deep breathing and Valsalva ratio reduced to < 50 % of minimal normal value | |
* original definition was >50%, this will result in error if the value is exactly equal to 50%.
Table 5. Calculation of cardiovagal score.
| Resultados | Degree of abnormality | Adrenergic score | |
| Value | Definition | ||
| Normal | 0 | ||
| Abnormal | Mild | 1 | Valsalva maneuver: Early phase 2 drop reduction < 40 >20* mmHg Or Late phase 2 does not return to baseline Or Pulse pressure reduction ≤ 50% of baseline Or Systolic pressure recovery time 4-5 seconds |
| Moderate | 2 | Valsalva maneuver: Early phase 2 reduction > 40 > 20 mmHg And Absent phase late phase 2 Or Absent phase 4 Or Systolic pressure recovery time 6-9 seconds |
|
| Severe | 3 | Tilt: OH (SBP reduction = 30 mm Hg; MBP = 20 mm Hg) (****) or Valsalva maneuver: Early phase 2 reduction = (**) 40 mmHg Plus Absent phase 2 Plus Absent phase 4 Or Absent Phases 2 and 4 and systolic pressure recovery time = 10 seconds (***) |
|
| 4 | Tilt + Valsalva maneuver: # 3 + OH (SBP reduction = 30 mm Hg; MBP = 20 mm Hg) |
||
*There are slightly different criteria for adrenergic failure as defined in 3 compared to a more recent text 5. I adopted * from the initial validated study 3. ** Changed from > to ≥ to remove ambiquity. *** The definition for the adrenergic score 3 differs in 3 and 5, hence I adopted definition in 3 that was expanded adding systolic pressure recovery time from 5. **** In original definition, the OH with normal Valsalva maneuver would be given score 0. Although rare (normal Valsalva maneuver + OH), this combination can be seen in a partial square variant of VM. Since OH signifies severe adrenergic impairment, the isolated OH is assigned to score 3.
Table 6. Calculation of adrenergic score
| Resultados | Degree of abnormality | Sudomotor score | |
| Value | Definition | ||
| Normal | 0 | ||
| Abnormal | Mild | 1 | Single site abnormal and ≥ 50 % of lower limit or Length dependent pattern* or Persistent sweat activity |
| Moderate | 2 | Single site < 50% of lower limit or Two or more sites reduced and ≥ 50 % of lower limit | |
| Severe | 3 | Two or more sites < 50% of lower limit | |
At least 3 sites should be studied. *Length dependent pattern in QSART is defined as reduction of the distal sweat volume more than 1/3 of proximal value. Text in bold has been added to improve clarity.
Table 7. Calculation of sudomotor score.
| Cardiovagal evaluation | ||
| Test | Resultados | Minimum of normal values* |
| Deep breathing [BPM] | 5 | 7 |
| Valsalva ratio | 1.35 | 1.51 |
| *normative data are adjusted for a gender and age of a patient | ||
| Adrenergic evaluation | |||||
| Test: Blood pressure responses to Valsalva maneuver | |||||
| Pressure [mmHg] | Baseline | Phase 2 | Pressure recovery time | Phase 4 | |
| Early | Late | ||||
| Systolic | 144.6 | 104.2 | 108 | 3.3 | 149 |
| Mean | 106 | 81.5 | 85.7 | n/a | 111.1 |
| Diastolic | 86.7 | 70.2 | 74.5 | n/a | 92.2 |
| Test: Tilt test | |||||
| Posição | HR [BPM] | SBP [mmHg] | DBP [mmHg] | ||
| Supine | 68 | 194 | 93 | ||
| Tilt [min] | 1 | 69 | 170 | 89 | |
| 2 | 70 | 165 | 89 | ||
| 3 | 70 | 161 | 87 | ||
| 4 | 71 | 159 | 88 | ||
| 5 | 69 | 152 | 86 | ||
| 6 | 72 | 155 | 85 | ||
| 7 | 70 | 148 | 86 | ||
| 8 | 71 | 142 | 82 | ||
| 9 | 71 | 136 | 82 | ||
| 10 | 71 | 138 | 82 | ||
| Orthostatic hypotension evaluation | |||||
| Pressure [mmHg] | Max drop of pressure compared to baseline | Duration of drop [min] | |||
| Systolic | 58 | 8 | |||
| Mean | 26.7 | n/a | |||
| Diastolic | 11 | n/a | |||
| Sudomotor Evaluation | ||||
| Test: Quantitative sudomotor axon reflex test (QSART) | ||||
| Location | Site (l/r) | Latency [min] | Volume | Minimum of normal volume* |
| Forearm | l | 2.3 | 2.487 | 0.3 |
| Proximal leg | l | 2.07 | 0.123 | 0.23 |
| Distal leg | l | 3.45 | 0.631 | 0.23 |
| Foot | l | 2.54 | 0.644 | 0.27 |
| *normative data are adjusted for a gender and age of a patient | ||||
| Composite Autonomic Severity Score | |||||||
| Cardiovagal | 1 | Adrenergic | 4 | Sudomotor | 1 | Total | 6 |
Table 8. An example of the results of the autonomic testing and corresponding CASS scores.

Figure 1 Recommended setup of the acquisition system. The screen is divided into raw and calculated data. HR= heart rate, SBP/DBP/MBP= systolic/diastolic/mean blood pressure, PP=pulse pressure, SBF/DBF/MBF = systolic/diastolic/mean blood flow velocity.

Figure 2 The screen is divided into 2 screens with long time scale (trend) and short time scale (details) of the same signals. This setting is particularly useful for prolonged tilt studies where both trend and immediate values are important.

Figure 3 Flexible setup of the data acquisition software. For example, it should be easy to add visible numerical values (as it is seen in three windows) or add/delete a channel.

Figure 4 Example of recording of Valsalva maneuver.

Figure 5 Calculation of RSA amplitude. The average RSA amplitude is equal to 21.9 that was obtained as follows: average RSA = [(89.2- 68.8) + (89.7-67.7) + (90.5-67.4) + (91.1-67.7) + (90.1-66.2) + (87.7-69.1)] / 6.

Figure 6 Normal response. The average RSA amplitude = 9.7 results obtained from a 55 year old man.

Figure 7 Moderately abnormal deep breathing test. The average RSA amplitude is equal to 3.2 Data obtained from a 54 year old man. The Valsalva ratio was normal.

Figure 8 Severely abnormal deep breathing test. The heart rate is fixed, the average RSA amplitude is equal to 0.6. This is equal to reduction by 91 % from the limit of normal value that is 7 bpm (Table 1). Data obtained from a 71 year old woman.
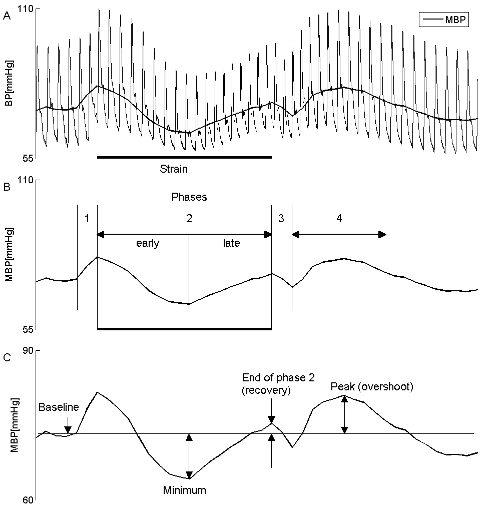

Figure 9. Typical blood pressure responses to VM in a healthy subject has 4 phases (A-B). Panels (C-E) show how to measure changes in BP during phase 2 and phase 4. Baseline blood pressure is obtained just before the VM. The pressure recovery time (PRT, F) is defined as a time interval (in seconds) that starts when the blood pressure is lowest in the phase 3 and ends when the blood pressure reaches the baseline. PRT is calculated from the systolic blood pressure, all remaining parameters are obtained from the mean blood pressure. MBP = mean blood pressure, SBP/DBP = systolic/diastolic blood pressure, PP= pulse pressure.

Figure 10. A square-wave variant of VM.

Figure 11. Valsalva ratio is defined as the maximum heart rate during the maneuver (121.2 mmHg) divided by the lowest heart rate (78.2 mm Hg) obtained within 30 seconds of the peak heart rate. In this example the Valsalva ratio is equal to 1.55 (= 121.2 / 78.2).

Figure 12. Normal VM. Both late phase 2 (100.2 mm Hg) and phase 4 (107.5 mmHg) exceed the baseline (96.8 mmHg).
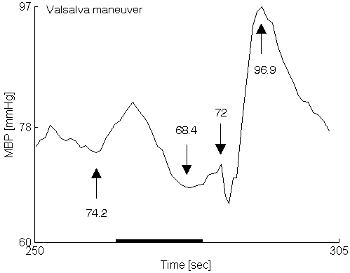
Figure 13. Mildly abnormal VM. The MBP at the end of phase 2 (72 mm Hg) failed to reach the baseline (74.2 mmHg).
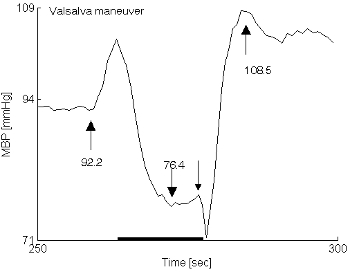
Figure 14. Moderately abnormal VM. There is an increased difference in MBP between the baseline and the end of phase 2 compared to Figure 13. Phase 4 is normal (108.5 mmHg).

Figure 15. Severely abnormal VM. The recovery of the MBP at the end of phase 2 and the phase 4 overshoot are missing. Note also supine hypertension that typically accompanies severe generalized autonomic failure.

Figure 16. Normal responses of heart rate and blood pressure to tilt.
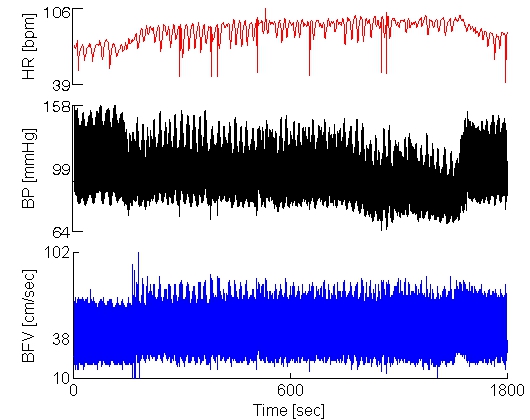
Figure 17. Mild orthostatic hypotension at the end of the tilt. Note that the blood flow is stable.

Figure 18. Severe progressive orthostatic hypotension during the tilt.

Figure 19. Mixed syncope. During the tilt, the excessive heart rate increment (1) was insufficient to prevent drop of the blood pressure (2) until the occurrence of vasovagal reaction (3) when patient lost consciousness.

Figure 20. Sweat capsule with tubing on the left, assembled capsule on the right.

Figure 21. Example of attachment of capsule to the skin using selfadhesive elastic wrap.

Figure 22. Stable baseline of spontaneoes sweating.
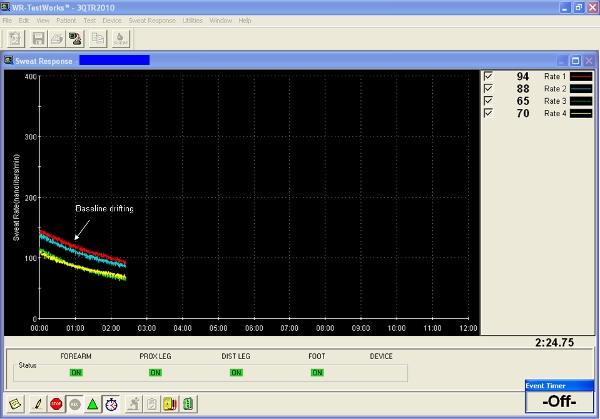
Figure 23. Drifting baseline of spontaneoes sweating.

Figure 24. Placement of markers of stimulation and recordings.

Figure 25. Principles of measurement of latency and sweat volume.

Figure 26. Normal QSART, CASS-sudomotor score= 0, 59 y/o man.

Figure 27. Persistent sweat activity, 31 y/o woman, this pattern usually signifies mild sudomotor impairment and can be seen in painful neuropathies or diabetes.
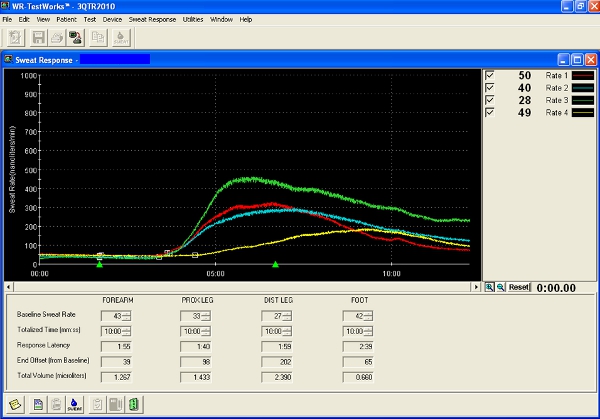
Figure 28. Mildly abnormal QSART,CASS-sudomotor =1. This test showed normal volumes but decrease of the distal sweat output that is consistent with length dependent pattern. 47 y/o woman.

Figure 29. Mildly abnormal QSART, CASS-sudomotor =1. The test showed reduced distal volume. 42 y/o woman.

Figure 30. Moderately abnormal, QSART CASS-sudomotor = 2. 64 y/o woman.
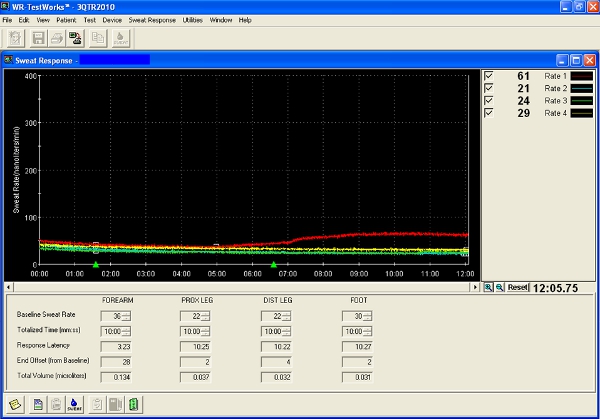
Figure 31. Severily abnormal QSART, CASS-sudomotor = 3. 56 y/o woman.
Discussion
Pitfalls
Completing the autonomic testing is in most of patients straightforward and can be done within 1 hours. Particular pitfalls of each step of testing is discussed below.
Equipment, data acquisition and processing of autonomic signals.
There are number of pitfalls related primarily to data quality. Inadequate cleaning of skin can lead to excessive noise in ECG signal that can render detection of R wave difficult. Improper placement of the blood pressure sensor my give false high or low values. Transcranial Doppler signal of high quality can be difficult to get in elderly patients due small bone window. Software for data processing may not be robust enough to distinguish artifacts at the blood pressure, for example in Parkinson patients with tremor.
Deep breathing
- Anxiety and abnormal respiratory pattern can affect the results of deep breathing. Subject should be well relaxed during the testing. A good marker of anxiety is the heart rate profile. If subject is anxious, the heart rate can be elevated. Before starting deep breathing test, make sure that the heart rate is not trending up or down, if this happened wait until the mean heart rate remains flat. The resting respiratory pattern should be normal, e.g there should be no hyperventilation (as measured by end tidal CO2) or tachypnea (respiratory rate is above 11 per minute).
- The deep breathing test has limited usefulness in certain cardiac dysrythmia for example in atrial fibrillation or when the heart rate is controlled by pacemaker because the vagal nerve modulation of the heart will be override by either the heart-generated rhythm or by a pacemaker. Basic knowledge of cardiac rhythm abnormalities is recommended.
- Improper detection of R waves due artifacts will obviously cause errors in results. This can happened if the R waves are too small to be reliably detected, or if the ECG background is noisy for example due poor skin contact.
Valsalva maneuver
Valsalva maneuver requires considerable cooperation from the subjects Many elderly or frail patients cannot perform the Valsalva maneuver correctly. Most common reason is weakness of the mouth muscles that results in air leak during the respiratory strain. In this case it is effective to gentle seal the air leak around the tube with fingers6.
Evaluation of adrenergic functions cannot be done in a square-wave variant of Valsalva maneuver (Figure 10). This response is rare but can be seen in healthy subjects or in patients with congestive heart failure.
Tilt testing
Number of medication can affect the tilt test rendering interpretation of the test difficult. It is not always practical to discontinue medication before testing.
It may be difficult to obtain good quality recordings in movement disorders patients, for example in Parkinson patients with tremor.
Sudomotor testing (QSART)
- Incomplete removal of oily surface or too much skin irritation can affect sweat output.
- Leaks if the capsule is not watertight or pain due too much tight capsule
- Commonly used medication has anticholinergic effect that interferes with the sweat test. In many cases, is in impractical to discontinue these medications rendering interpretation of results difficult.
Grading of autonomic impairment using the Composite Autonomic Severity Score (CASS).
Generation of CASS score is quite cumbersome because it involves multiple comparisons in both absolute and percent values. Unfortunately, there is no commercial software that enables to calculate the score automatically. At UMASS, we use proprietary software that generates the CASS score automatically. Example of CASS scores is on the Table 8.
Declarações
The authors have nothing to disclose.
Acknowledgements
Author thanks to Dr. Lan Qin and Shane Stanek for help with collection of data.
Materials
Table 9 Recommended equipment.
| Name of the equipment | Company | Comments |
| Motorized tilt table | WR Medical Electronic | Any table with smooth movement reaching 70 degree within 5-10 seconds |
| ECG monitor | Any device with analog output | |
| Noninvasive beat-to-beat blood pressure monitor | Finapres Medical Systems | Several models are available, all are similar |
| Q-Sweat | WR Medical Electronic | |
| Transcranial Doppler | Any device with analog output | |
| Recording system | LabChart, ADInstruments | Simple programming |
| Recording system | Labview | Complex programming |
| Recording system | Matlab | Complex programming |
| Recording system | WR Medical | Ready to use, but limited flexibility |
| CO2 monitor | Many models used for sleep studies | |
| Respiratory monitor | Simple thermistor attached to a recording system |
Referências
- Low, P. A., Denq, J. C., Opfer-Gehrking, T. L., Dyck, P. J., O’Brien, P. C., Slezak, J. M. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve. 20, 1561-1568 (1997).
- Low, P. A., Denq, J. C., Opfer-Gehrking, T. L., Dyck, P. J., O’Brien, P. C., Slezak, J. Effect of age and gender on sudomotor and cardiovagal function and blood pressure response to tilt in normal subjects. Muscle Nerve. 20, 1561-1568 (1997).
- Low, P. A. Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc. 68, 748-752 (1993).
- Low, P. A., Low, P. A. Laboratory evaluation of autonomic function. Clinical Autonomic disorders. , 179-209 (1997).
- Low, P. A., Low, P. A. Laboratory evaluation of autonomic failure. Clinical Autonomic disorders. , 179-209 (2008).
- Novak, P. Assessment of sympathetic index from Valsalva maneuver. Neurology. , (2011).

