Motor Maps
26,962 Views
•
•
Overview
Source: Laboratories of Jonas T. Kaplan and Sarah I. Gimbel—University of Southern California
One principle of brain organization is the topographic mapping of information. Especially in sensory and motor cortices, adjacent regions of the brain tend to represent information from adjacent parts of the body, resulting in maps of the body expressed on the surface of the brain. The primary sensory and motor maps in the brain surround a prominent sulcus known as the central sulcus. The cortex anterior to the central sulcus is known as the precentral gyrus and contains the primary motor cortex, while the cortex posterior to the central sulcus is known as the postcentral gyrus and contains the primary sensory cortex (Figure 1).
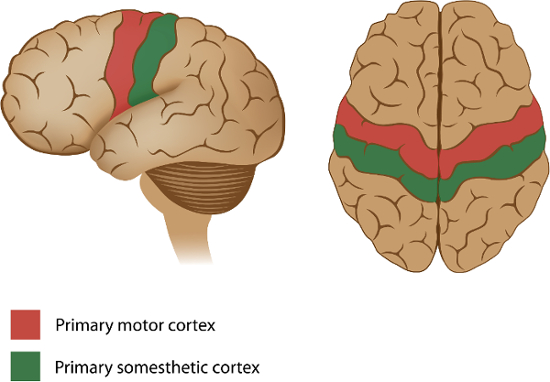
Figure 1: Sensory and motor maps around the central sulcus. The primary motor cortex, which contains a motor map of the body's effectors, is anterior to the central sulcus, in the precentral gyrus of the frontal lobe. The primary somesthetic (sensory) cortex, which receives touch, pain, and temperature information from the external parts of the body, is located posterior to the central sulcus, in the postcentral gyrus of the parietal lobe.
In this experiment, functional neuroimaging is used to demonstrate the motor map in the precentral gyrus. This map is often called the motor homunculus, which is Latin for "little man," because it is as if there is a little version of one's self represented in this part of a person's brain. One interesting property of this map is that more cortical space is devoted to body parts requiring finer control, such as the hands and mouth, which results in disproportionate representation of those appendages in the cortex. Also, because of the anatomy of the motor system, the neurons that control the right side of the body are in the left primary motor cortex, and vice versa. Therefore, when a participant in the experiment is asked to move their right hand or foot, an increased activation on their left precentral gyrus is expected.
In this experiment, participants are asked to alternately move their hands and feet, on the left and right sides, while their brain activity is measured with fMRI. Since the fMRI signal relies on changes in blood oxygenation, which are slow in comparison to the movements the participants make, the periods of movement are separated with periods of stillness to ensure that the various conditions can be distinguished from each other and from the resting baseline. To achieve precise timing of the movements, participants are instructed on when to begin and end each movement with a visual cue. The methods in this video are similar to those used by several fMRI studies that have demonstrated somatotopy in primary motor cortex.1,2
Procedure
1. Recruit 20 participants.
- Confirm that the participants have no history of neurological or psychological disorders.
- Confirm that the participants are all right-handed using the handedness questionnaire.
- To ensure the participants can see the visual cues properly, make sure they have normal or corrected to normal vision.
- Make sure the participants have no metal in their body. This is an important safety requirement due to the high magnetic field involved in fMRI.
- Since the fMRI requires lying in the small space of the scanner bore, confirm that the participants don't suffer from claustrophobia.
2. Pre-scan procedures
- Fill out the pre-scan paperwork.
- When participants come in for their fMRI scan, have them first fill out a metal screen form to make sure they have no counter-indications for MRI, an incidental findings form giving consent for their scan to be looked at by a radiologist, and a consent form detailing the risks and benefits of the study.
- Have the participants remove all metal from their body (including belts, wallets, phones, hair clips, coins, and all jewelry) to prepare to go in the scanner.
3. Provide instructions for the participant.
- Tell the participant that when they see a hand on the screen, they are to begin moving their hand until the visual cue disappears. Inform the participant that the hand movement involves touching the thumb to each finger of the same hand in order and repeating this sequence in reverse. When the cue appears on the left side of the screen, they are to move their left hand, and when the cue appears on the right side of the screen, they are to move their right hand.
- Tell the participant that when they see a foot on the screen, they are to begin moving their foot and continue to do so until the visual cue disappears. Inform the participant that the foot movement involves repetitively pressing the foot down, as if pressing on an imaginary pedal. When the cue appears on the left side of the screen, they are to move their left foot, and when the cue appears on the right side of the screen, they are to move their right foot.
- Stress to the participant the importance of keeping their head still, even while they are moving their hand or foot.
4. Guide the participant into the scanner.
- Give the participant earplugs (to protect their ears from the noise of the scanner) and earphones (to wear so they can hear the experimenter during the scan), and have them lie down on the bed with their head in the coil.
- Give the participant the emergency squeeze ball and instruct them to squeeze it in case of emergency during the scan.
- Secure the participant's head in the coil with foam pads to avoid excess movement during the scan, and remind the participant that it is very important to stay as still as possible during the scan, as even the smallest movements blur the images.
5. Data collection
- Collect a high-resolution anatomical scan.
- Begin functional scanning.
- Synchronize the start of the stimulus presentation with the start of the scanner.
- Present the visual cues via a laptop connected to a projector. The participant should have a mirror above their eyes, reflecting a screen at the back of the scanner bore.
- Present each visual cue for 12 s, followed by 12 s of resting baseline. Alternate between the left hand, right hand, left foot, and right foot.
- Repeat four repetitions of each condition, for a total of 6.5 min.
6. Post-scan procedures
- Bring the participant out of the scanner.
- Debrief the participant.
- Pay the participant.
7. Data analysis
- Preprocess the data.
- Perform motion correction to reduce motion artifacts.
- Perform temporal filtering to remove signal drifts.
- Smooth the data to increase signal-to-noise ratio.
- Model the data for each participant.
- Create a model of what the expected hemodynamic response should be for each task condition.
- Fit the data to this model, resulting in a statistical map, where the value at each voxel represents the extent to which that voxel was involved in the task condition.
- Register the participant's brain to a standard atlas in order to combine data across participants.
- Combine statistical maps across subjects for a group level analysis of the data.
Motor information is organized according to anatomical divisions in the primary motor cortex, creating a topographical map in the brain.
Located in the precentral gyrus, cortical representations of the body are organized into a motor homunculus—”little man”—and are arranged in an inverted manner, such that the areas that control the toes are found in the medial wall and the tongue is located near the lateral sulcus.
Furthermore, body parts that require finer voluntary motor control, such as the hands and their associated digits, have larger representations in the cortex, compared to anatomical features that don’t require such precise manipulation—like the hip.
The homunculus is also lateralized, with neurons in the left primary motor cortex—shown here—controlling the right side of the body, and vice versa. Thus, when an individual moves their right hip, there is increased cortical activation on their left precentral gyrus within a discrete region.
This video details an experiment that uses modern functional neuroimaging to demonstrate the body-mapped organization of the human primary motor cortex, including how to collect and analyze brain activity when participants move their hands or feet.
In this experiment, brain activity is measured using functional magnetic resonance imaging, abbreviated as fMRI, while participants are repetitively cued to move different body parts—like the digits on their left or right hands.
This technique relies on changes in blood oxygenation levels, referred to as the BOLD—Blood-Oxygenation-Level-Dependent—response. For an in-depth look at the principles behind the method, please refer to another video in JOVE’s SciEd Essentials of Neuroscience Collection, fMRI: Functional Magnetic Resonance Imaging.
In the context presented here, when a body part, such as the left foot, is flexing back and forth, oxygenated cerebral blood flow—supplied by arteries in the brain—increases to neural regions that are active during this movement, like the primary motor cortex.
However, this hemodynamic response occurs more slowly than the actual physical motion, which warrants that actions be separated with periods of rest.
Thus, each body movement is precisely timed to distinguish the four conditions from one another: left hand, left foot, right hand, and right foot.
For example, participants in a fMRI machine are asked to start gesturing their left hand when one appears on the left side of a presentation screen.
The required hand movement is actually complex, and involves touching the thumb to each finger, in order, starting with the pointer. Then, the participant must repeat these actions in the opposite direction, starting with the pinky.
Movement is stopped when the cue—in this instance, the picture of the left hand—disappears from the screen.
Likewise, when they see a foot on the right, they are instructed to move their right foot by pushing it down repeatedly, until the image disappears.
Here, the dependent variable is the intensity of the BOLD response after a movement from the hand or foot, which can then be localized to specific brain regions.
For a left hand movement, brain activation is primarily expected on the right dorsolateral surface of the precentral gyrus. In contrast, for a right hand movement, brain activation is anticipated on the left dorsolateral surface. These results would align with the lateralized motor homunculus.
Prior to the experiment, recruit participants who are right-handed, have normal or corrected-to-normal vision, do not have any metallic implants in their body, or suffer from claustrophobia on account of experimental control and safety concerns.
Have them fill out pre-scan paperwork, which includes questions related to health and safety issues during the session, such as consent for a radiologist to look at their images in the case of incidental findings, as well as detailing the risks and benefits of the study.
Ask the participant to also remove all metal objects from their body—including watches, phones, wallets, keys, belts, and coins—to prepare for entering into the scanning room.
Next, explain the task rules: the appendage they need to move—in this case their foot—will appear as a visual cue on the corresponding side of the screen. Demonstrate how they should move their foot by repeatedly pressing it down, as if pushing on an imaginary pedal.
When a hand cue appears, they must touch the thumb to each finger of the same hand in order and then repeat this sequence in reverse.
Now, bring the participant into the imaging room. Provide earplugs to protect their ears from loud noises and earphones so that they can hear any additional communication during the session. Have them lie down on the bed with their head in the coil and secure it with foam pads to avoid excess movement and blur during the scan.
Above the participants’ eyes, place a mirror that reflects a screen at the back of the scanner bore. Then, give them a squeeze ball to use in case of emergency. Also remind them that it is very important to stay as still as possible the entire time.
After guiding the participant inside the machine, first collect high-resolution, anatomical images. To begin the functional portion, synchronize the stimulus presentation with the start of the scanner.
Present the visual cues via a laptop connected to a projector, each for 12 s, followed by 12 s of resting baseline. Alternate between the four conditions: left hand, right hand, left foot, and right foot—repeating each four times within 6.5 min.
Once the scan is completed, direct the participant out of the room. Debrief them and provide compensation for their participation in the study.
As the first step of the analysis, preprocess the data by performing motion correction to reduce artifacts, temporal filtering to remove signal drifts, and spatial smoothing to increase the signal-to-noise ratio.
Using these data, create a model of the expected hemodynamic response for each task condition. Then, fit the data to this model, resulting in a statistical map for each subject, where the value at each voxel—a 3D pixel of volume—represents the extent to which that voxel was involved in the task condition.
Register the participant’s brain to a standard atlas in order to combine data across each participant. Then, combine all statistical maps across participants for a group level analysis. Note that changes in blood flow are represented by different colors on the surface of the brain.
Movements of the right hand, shown in blue, produced the greatest activation on the left lateral surface of the precentral gyrus, whereas engaging the left hand, represented in green, produced the greatest activation on the right lateral surface.
Additionally, flexing the right foot, indicated by light blue, produced activation on the left medial surface, while the greatest activation for left foot movements, in yellow, were on the right medial surface.
These results suggest that motor actions can be localized to discrete regions of the primary motor cortex in both hemispheres, supporting the motor homunculus.
Now that you are familiar with executing an fMRI experiment to observe the organization of the primary motor cortex, let’s consider how the brain manages movement after damage, or after the attachment of prosthetic limbs.
Damage to the left precentral gyrus, such as from a stroke, can lead to difficulty in moving the right side of the body.
As you’ve learned in this video, the specific parts that are impacted depend upon the extent of injury: impairments could be small and affect a single finger, or large enough to influence all of the digits and the entire arm.
While the representations seem straightforward, the primary motor cortex does not work alone, as it’s just a segment within a wider network of regions that are involved in the selection, planning, and coordination of movement. Thus, localizing damage may not be as easy as it seems.
One potential therapeutic approach for improving limb function in amputees involves brain-computer interfaces. This technically advanced method is based on electromyographic, or EMG signals—the electrical communication between motor neurons and muscle movements.
Researchers are developing ways to integrate EMG recordings with limb prostheses to more seamlessly control motor behaviors, like standing, or even walking up a ramp.
You’ve just watched JoVE’s introduction to motor maps. Now you should have a good understanding of how to design and conduct the fMRI experiment, and finally how to analyze and interpret the brain activation results.
Thanks for watching!
Results
In this experiment, researchers measured brain activity with fMRI, while participants moved their hands or feet. Statistical analysis of the changes in blood flow is represented by different colors on the surface of the standard atlas brain. The colors identify the voxels, whose time course best matched the predicted time course for a specific condition.
The results demonstrate different activation foci within the precentral gyrus for the movement of the different limbs (Figure 2). Movement of the right hand produced the greatest activation on the left lateral surface of the gyrus (blue), while movement of the left hand produced the greatest activation on the right lateral surface (green). When participants moved their feet, activation was greatest where the precentral gyrus extends around to the medial surface of the brain. Right-sided foot movements produced activation on the left medial surface (cyan), while the greatest activation for left foot movements was on the right medial surface (yellow).
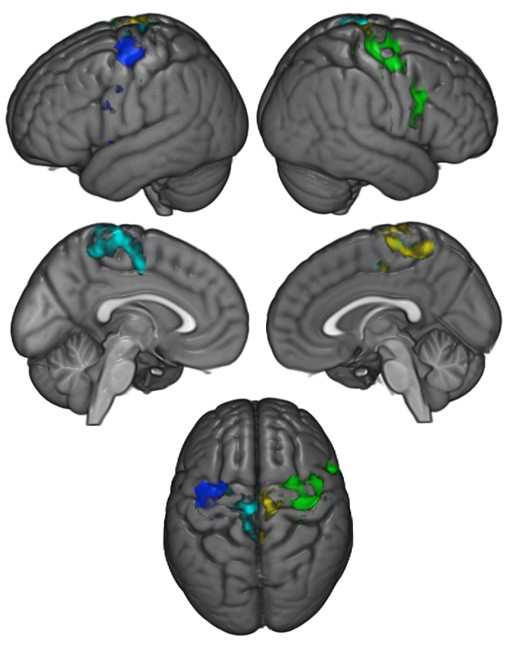
Figure 2: Brain activations resulting from movement of the hands and feet across participants. Blue = Movement of the right hand; Green = Movement of the left hand; Cyan = Movement of the right foot; Yellow = Movement of the left foot.
Applications and Summary
These results demonstrate the somatotopic, or body-mapped organization of the human primary motor cortex. This mapping has implications for how damage to the brain affects movement. For example, damage to the left precentral gyrus leads to difficulty in moving the right side of the body, and the specific parts of primary motor cortex affected can lead to problems in controlling specific parts of the body. However, it is also important to note that the primary motor cortex is only one of many brain regions involved in the control of movement. The precentral gyrus is part of a wider network of brain regions that participate in the selection, planning, and coordination of movement.
The ability to measure effector-specific activity in motor cortex also leads to the possibility of brain-computer interfaces, such as those that allow control of prosthetic limbs. For example, using direct recordings of neurons in the primary motor cortex, researchers have demonstrated that monkeys can control a prosthetic limb to feed themselves.3
References
- Lotze, M., et al. fMRI evaluation of somatotopic representation in human primary motor cortex. Neuroimage 11, 473-481 (2000).
- Rao, S.M., et al. Somatotopic mapping of the human primary motor cortex with functional magnetic resonance imaging. Neurology 45, 919-924 (1995).
- Velliste, M., Perel, S., Spalding, M.C., Whitford, A.S. & Schwartz, A.B. Cortical control of a prosthetic arm for self-feeding. Nature 453, 1098-1101 (2008).
Transcript
Motor information is organized according to anatomical divisions in the primary motor cortex, creating a topographical map in the brain.
Located in the precentral gyrus, cortical representations of the body are organized into a motor homunculus—”little man”—and are arranged in an inverted manner, such that the areas that control the toes are found in the medial wall and the tongue is located near the lateral sulcus.
Furthermore, body parts that require finer voluntary motor control, such as the hands and their associated digits, have larger representations in the cortex, compared to anatomical features that don’t require such precise manipulation—like the hip.
The homunculus is also lateralized, with neurons in the left primary motor cortex—shown here—controlling the right side of the body, and vice versa. Thus, when an individual moves their right hip, there is increased cortical activation on their left precentral gyrus within a discrete region.
This video details an experiment that uses modern functional neuroimaging to demonstrate the body-mapped organization of the human primary motor cortex, including how to collect and analyze brain activity when participants move their hands or feet.
In this experiment, brain activity is measured using functional magnetic resonance imaging, abbreviated as fMRI, while participants are repetitively cued to move different body parts—like the digits on their left or right hands.
This technique relies on changes in blood oxygenation levels, referred to as the BOLD—Blood-Oxygenation-Level-Dependent—response. For an in-depth look at the principles behind the method, please refer to another video in JOVE’s SciEd Essentials of Neuroscience Collection, fMRI: Functional Magnetic Resonance Imaging.
In the context presented here, when a body part, such as the left foot, is flexing back and forth, oxygenated cerebral blood flow—supplied by arteries in the brain—increases to neural regions that are active during this movement, like the primary motor cortex.
However, this hemodynamic response occurs more slowly than the actual physical motion, which warrants that actions be separated with periods of rest.
Thus, each body movement is precisely timed to distinguish the four conditions from one another: left hand, left foot, right hand, and right foot.
For example, participants in a fMRI machine are asked to start gesturing their left hand when one appears on the left side of a presentation screen.
The required hand movement is actually complex, and involves touching the thumb to each finger, in order, starting with the pointer. Then, the participant must repeat these actions in the opposite direction, starting with the pinky.
Movement is stopped when the cue—in this instance, the picture of the left hand—disappears from the screen.
Likewise, when they see a foot on the right, they are instructed to move their right foot by pushing it down repeatedly, until the image disappears.
Here, the dependent variable is the intensity of the BOLD response after a movement from the hand or foot, which can then be localized to specific brain regions.
For a left hand movement, brain activation is primarily expected on the right dorsolateral surface of the precentral gyrus. In contrast, for a right hand movement, brain activation is anticipated on the left dorsolateral surface. These results would align with the lateralized motor homunculus.
Prior to the experiment, recruit participants who are right-handed, have normal or corrected-to-normal vision, do not have any metallic implants in their body, or suffer from claustrophobia on account of experimental control and safety concerns.
Have them fill out pre-scan paperwork, which includes questions related to health and safety issues during the session, such as consent for a radiologist to look at their images in the case of incidental findings, as well as detailing the risks and benefits of the study.
Ask the participant to also remove all metal objects from their body—including watches, phones, wallets, keys, belts, and coins—to prepare for entering into the scanning room.
Next, explain the task rules: the appendage they need to move—in this case their foot—will appear as a visual cue on the corresponding side of the screen. Demonstrate how they should move their foot by repeatedly pressing it down, as if pushing on an imaginary pedal.
When a hand cue appears, they must touch the thumb to each finger of the same hand in order and then repeat this sequence in reverse.
Now, bring the participant into the imaging room. Provide earplugs to protect their ears from loud noises and earphones so that they can hear any additional communication during the session. Have them lie down on the bed with their head in the coil and secure it with foam pads to avoid excess movement and blur during the scan.
Above the participants’ eyes, place a mirror that reflects a screen at the back of the scanner bore. Then, give them a squeeze ball to use in case of emergency. Also remind them that it is very important to stay as still as possible the entire time.
After guiding the participant inside the machine, first collect high-resolution, anatomical images. To begin the functional portion, synchronize the stimulus presentation with the start of the scanner.
Present the visual cues via a laptop connected to a projector, each for 12 s, followed by 12 s of resting baseline. Alternate between the four conditions: left hand, right hand, left foot, and right foot—repeating each four times within 6.5 min.
Once the scan is completed, direct the participant out of the room. Debrief them and provide compensation for their participation in the study.
As the first step of the analysis, preprocess the data by performing motion correction to reduce artifacts, temporal filtering to remove signal drifts, and spatial smoothing to increase the signal-to-noise ratio.
Using these data, create a model of the expected hemodynamic response for each task condition. Then, fit the data to this model, resulting in a statistical map for each subject, where the value at each voxel—a 3D pixel of volume—represents the extent to which that voxel was involved in the task condition.
Register the participant’s brain to a standard atlas in order to combine data across each participant. Then, combine all statistical maps across participants for a group level analysis. Note that changes in blood flow are represented by different colors on the surface of the brain.
Movements of the right hand, shown in blue, produced the greatest activation on the left lateral surface of the precentral gyrus, whereas engaging the left hand, represented in green, produced the greatest activation on the right lateral surface.
Additionally, flexing the right foot, indicated by light blue, produced activation on the left medial surface, while the greatest activation for left foot movements, in yellow, were on the right medial surface.
These results suggest that motor actions can be localized to discrete regions of the primary motor cortex in both hemispheres, supporting the motor homunculus.
Now that you are familiar with executing an fMRI experiment to observe the organization of the primary motor cortex, let’s consider how the brain manages movement after damage, or after the attachment of prosthetic limbs.
Damage to the left precentral gyrus, such as from a stroke, can lead to difficulty in moving the right side of the body.
As you’ve learned in this video, the specific parts that are impacted depend upon the extent of injury: impairments could be small and affect a single finger, or large enough to influence all of the digits and the entire arm.
While the representations seem straightforward, the primary motor cortex does not work alone, as it’s just a segment within a wider network of regions that are involved in the selection, planning, and coordination of movement. Thus, localizing damage may not be as easy as it seems.
One potential therapeutic approach for improving limb function in amputees involves brain-computer interfaces. This technically advanced method is based on electromyographic, or EMG signals—the electrical communication between motor neurons and muscle movements.
Researchers are developing ways to integrate EMG recordings with limb prostheses to more seamlessly control motor behaviors, like standing, or even walking up a ramp.
You’ve just watched JoVE’s introduction to motor maps. Now you should have a good understanding of how to design and conduct the fMRI experiment, and finally how to analyze and interpret the brain activation results.
Thanks for watching!
