‘Bioluminescent’ Reporter Phage for the Detection of Category A Bacterial Pathogens
Özet
A simple method for the identification of priority bacterial pathogens is to use genetically engineered reporter phage. These reporter phage, which are specific to their particular host species, are capable of rapidly transducing a bioluminescent signal response to host cells. Herein, we describe the use of reporter phage for the detection of Yersinia pestis.
Abstract
Yersinia pestis and Bacillus anthracis are Category A bacterial pathogens that are the causative agents of the plague and anthrax, respectively 1. Although the natural occurrence of both diseases' is now relatively rare, the possibility of terrorist groups using these pathogens as a bioweapon is real. Because of the disease's inherent communicability, rapid clinical course, and high mortality rate, it is critical that an outbreak be detected quickly. Therefore methodologies that provide rapid detection and diagnosis are essential to ensure immediate implementation of public health measures and activation of crisis management.
Recombinant reporter phage may provide a rapid and specific approach for the detection of Y. pestis and B. anthracis. The Centers for Disease Control and Prevention currently use the classical phage lysis assays for the confirmed identification of these bacterial pathogens 2-4. These assays take advantage of naturally occurring phage which are specific and lytic for their bacterial hosts. After overnight growth of the cultivated bacterium in the presence of the specific phage, the formation of plaques (bacterial lysis) provides a positive identification of the bacterial target. Although these assays are robust, they suffer from three shortcomings: 1) they are laboratory based; 2) they require bacterial isolation and cultivation from the suspected sample, and 3) they take 24-36 h to complete. To address these issues, recombinant "light-tagged" reporter phage were genetically engineered by integrating the Vibrio harveyi luxAB genes into the genome of Y. pestis and B. anthracis specific phage 5-8. The resulting luxAB reporter phage were able to detect their specific target by rapidly (within minutes) and sensitively conferring a bioluminescent phenotype to recipient cells. Importantly, detection was obtained either with cultivated recipient cells or with mock-infected clinical specimens 7.
For demonstration purposes, here we describe the method for the phage-mediated detection of a known Y. pestis isolate using a luxAB reporter phage constructed from the CDC plague diagnostic phage ΦA1122 6,7 (Figure 1). A similar method, with minor modifications (e.g. change in growth temperature and media), may be used for the detection of B. anthracis isolates using the B. anthracis reporter phage Wβ::luxAB 8. The method describes the phage-mediated transduction of a biolumescent phenotype to cultivated Y. pestis cells which are subsequently measured using a microplate luminometer. The major advantages of this method over the traditional phage lysis assays is the ease of use, the rapid results, and the ability to test multiple samples simultaneously in a 96-well microtiter plate format.
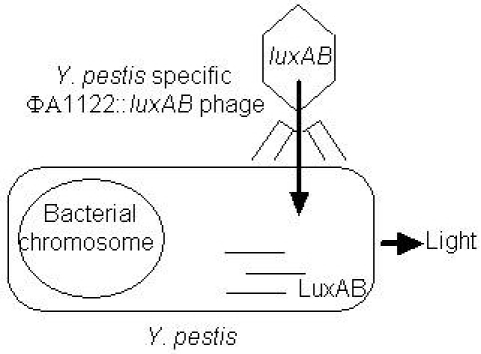
Figure 1. Detection schematic. The phage are mixed with the sample, the phage infects the cell, luxAB are expressed, and the cell bioluminesces. Sample processing is not necessary; the phage and cells are mixed and subsequently measured for light.
Protocol
1. Y. pestis plate inoculation
- Streak Y. pestis A1122 (BeiResources # NR15) stock cultures onto Luria-Bertani (LB) agar (Miller). Use sterile technique and perform all Y. pestis manipulations in a class II type A biosafety cabinet. Y. pestis A1122 is a BioSafety Level (BSL) 2 excluded select agent strain. It lacks both the 75 kb pair low-calcium response (Lcr) virulence plasmid, and the pgm locus that are required for virulence. Grow Y. pestis at 28°C for 48 h in a static temperature controlled air incubator. The growth rate of Y. pestis is slow with a generation time of 1.25 h 9.
2. Y. pestis liquid media inoculation
- Transfer a single Y. pestis colony into a sterile 17 x 100 mm culture tube containing 2 mL of LB broth using a sterile metal inoculation loop. Select a colony that is uniform in size, is indicative of the other colonies, and is clearly separated from the rest of the colonies on the plate. Vortex tube briefly and grow culture at 28°C for approximately 20 h in a shaking incubator (225 rpm).
3. Y. pestis outgrowth, reporter phage addition, and bioluminescent detection
- Dilute the overnight Y. pestis culture 1:20 into fresh LB broth in a 50 mL falcon tube (e.g., 500 μL of cells into 9.5 mL of medium) and grow at 28°C with shaking (225 rpm). Grow until an optical density at 600 nm (A600) of 0.2 is reached (approximately 5 h). Actively growing cells are preferable for detection since the ability of the phage to transduce a bioluminescent response is correlated to the viability and fitness of the host bacteria. Nevertheless, the detection system has been shown to be compatible with cells harvested at all stages of the growth cycle 7.
- Generate the substrate necessary for the bioluminescent reaction by preparing a 2% n-decanal solution. Mix 200 μL of n-decanal with 9.8 mL of LB broth. Vortex vigorously for 5 s. Prime the microplate luminometer injector with 2 mL of the 2% n-decanal solution. Pre-set the luminometer to autoinject 67 μL of the decanal solution to each microplate well and then immediately read the sample for 10 s.
- Dispense 1 mL aliquots of LB broth into 3 culture tubes. Add 20 μL of the reporter phage stock solution (stock of 5 x 109 plaque forming units [PFU]/mL) to each tube; the phage and media alone samples serves as a negative control. In the absence of Y. pestis cells, the addition of the reporter phage should not elicit a bioluminescent response.
- Dispense 1 mL aliquots of the Y. pestis culture (from step 3.1) into 6 culture tubes. Add 20 μL of the reporter phage stock to 3 of the cultures (test cultures). The remaining 3 cultures serve as a ‘cells alone’ negative control (background autobioluminescence). Mix cultures by vortexing briefly, and harvest 200 μL from each sample (for the time 0 read) and dispense into a white 96-well microtiter plate. Incubate the remaining culture at 28°C with shaking (225 rpm).
- Measure the time 0 samples for bioluminescence (relative light units, RLU) using the microplate luminometer.
- Harvest 200 μL of each sample after 10, 20, 30, 40, 50, and 60 min post-reporter phage addition, and measure the sample for bioluminescence. If Y. pestis cells are present, the reporter phage will specifically bind to the cell, inject its DNA, and use the hosts transcriptional and translational machinery to transcribe and translate the luxAB reporter genes (Figure 1).
- The strength of signal and the signal response time is proportional to the number of cells present. At high concentrations of cells (105-108 CFU/mL), a significant increase in RLU compared to the controls should be evident within 20 min. At lower cell concentrations, (102-104 CFU/mL), a significant increase in RLU should be evident within 40-60 min.
- Alternatively, to expedite the detection process without the need for Y. pestis outgrowth, a colony from a freshly grown plate may be mixed (by vortexing) directly in a 1.5 mL eppendorf tube with 200 μL of LB broth harboring the reporter phage. Dispense the cell/phage mixture into a well of a microtiter plate. Incubate the microtiter plate at 28°C and read the sample for bioluminescence after 60 min (single time point only).
4. Representative results:
A representative time course experiment of reporter phage mediated detection of Y. pestis is depicted in Figure 2. The negative controls of 1) phage alone (no cells), or 2) cells alone (no phage) provide baseline levels of bioluminescence of approximately 20 RLU throughout the 60 min incubation (baseline levels are luminometer specific). In contrast, an increase in bioluminescence for the test samples (reporter phage and cells) is evident at 15 min after phage addition. The signal strength should increase steadily over 60 min. Incubations for prolonged time periods (over 80 min), will result in a signal that will decline from the peak signal due to phage mediated lysis of host cells. Similar results are obtained at incubation temperatures of 37°C even though the optimum temperature for Y. pestis growth is 28°C 9.
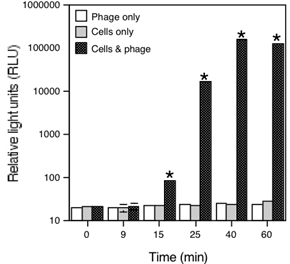
Figure 2. Phage-mediated bioluminescent detection of Y. pestis. At time 0, reporter phage and cells were mixed, incubated at 28°C, and bioluminescence (RLU) was monitored over time. A significant increase in RLU (* Students t-test, p<0.05) is evident within 15 min.
Discussion
This method demonstrates the ability of the reporter phage to rapidly detect Y. pestis since the reporter phage can transduce a bioluminescent signal response to cultured Y. pestis cells within 20 min after phage addition. The reporter phage is also capable of directly detecting Y. pestis in clinical matrices, without the prerequisite of isolation and subsequent cultivation 7. Compared to the standard phage lysis assays which generally require 48 h for completion, this significantly decreases the time to detection.
Previous studies have demonstrated that the wild-type ΦA1122 phage can lyse nearly all natural Y. pestis isolates, and is ‘specific’ for Y. pestis 6,10,11; however, some Y. pseudotuberculosis strains have been shown to be ΦA1122 susceptible when grown at temperatures above 20°C 6,10,12. The reason for the temperature-sensitive differential susceptibility is unknown, but presumably due to temperature-dependent changes in the cell surface layers/composition. Therefore, a potential caveat of the reporter phage detection system is the possibility of a false-positive response with strains from the closely-related species Y. pseudotuberculosis. Performing the reporter phage assay at the restrictive temperature (20°C) will prevent a false positive signal in samples that may contain Y. pseudotuberculosis. Thus, specificity can be strictly controlled when using isolated cultures grown at a specific temperature.
In summary, rapid detection and diagnosis of Y. pestis is essential for a positive prognosis since the plague, especially pneumonic plague, is nearly always fatal if treatment is not administered within the first 24 h after symptom onset. This method has the potential to meet these needs for the confirmed identification of cultured isolates or within clinically relevant matrices.
Açıklamalar
The authors have nothing to disclose.
Acknowledgements
This research was supported by the Small Business Innovation Research program of the National Institutes of Health (NIAID, 1R43AI082698-01) and the USDA National Institute of Food and Agriculture (NIFA, 2009-33610-20028).
Materials
| Name of the reagent | Company | Catalogue number |
|---|---|---|
| Difco LB agar, Miller | VWR | 90003-346 |
| Difco LB broth, Miller | VWR | 90003-350 |
| 17 x 100 mm culture tubes | USA Scientific | 1485-0810 |
| n-Decanal | Sigma | D7384 |
| Veritas microplate luminometer | Turner Biosystems | 9100-001 |
| Microlite microtiter 96-well plate | VWR | 62402-984 |
Referanslar
- Darling, R. G., Catlett, C. L., Huebner, K. D., Jarrett, D. G. Threats in bioterrorism. I: CDC category A agents. Emerg Med Clin North Am. 20, 273-309 (2002).
- Chu, M. C. . Laboratory manual of plague diagnostic tests.. , (2000).
- . . , (1999).
- Inglesby, T. V. Anthrax as a biological weapon, 2002: updated recommendations for management. JAMA. 287, 2236-2252 (2002).
- Schuch, R., Fischetti, V. A. Detailed genomic analysis of the Wbeta and gamma phages infecting Bacillus anthracis: implications for evolution of environmental fitness and antibiotic resistance. J Bacteriol. 188, 3037-3051 (2006).
- Garcia, E. The genome sequence of Yersinia pestis bacteriophage phiA1122 reveals an intimate history with the coliphage T3 and T7 genomes. J Bacteriol. 185, 5248-5262 (2003).
- Schofield, D. A., Molineux, I. J., Westwater, C. Diagnostic bioluminescent phage for detection of Yersinia pestis. Journal of Clinical Microbiology. 47, 3887-3894 (2009).
- Schofield, D. A., Westwater, C. Phage-mediated bioluminescent detection of Bacillus anthracis. Journal of Applied Microbiology. 107, 468-478 (2009).
- Chu, M. C. . CDC: Basic laboratory protocols for the presumptive identification of Yersinia pestis. , 1-19 (2001).
- Gunnison, J. B., Larson, A., Lazarus, A. S. Rapid differentiation between Pasteurella pestis and Pasteurella pseudotuberculosis by action of bacteriophage. J Infect Dis. 88, 254-255 (1951).
- Lazarus, A. S., Gunnison, J. B. The Action of Pasteurella pestis Bacteriophage on Strains of Pasteurella, Salmonella, and Shigella. J Bacteriol. 53, 705-714 (1947).
- Sergueev, K. V., He, Y., Borschel, R. H., Nikolich, M. P., Filippov, A. A. Rapid and sensitive detection of Yersinia pestis using amplification of plague diagnostic bacteriophages monitored by real-time PCR. PLoS One. 5, e11337-e11337 (2010).

