Detection of Toxin Translocation into the Host Cytosol by Surface Plasmon Resonance
概要
In this report, we describe how surface plasmon resonance is used to detect toxin entry into the host cytosol. This highly sensitive method can provide quantitative data on the amount of cytosolic toxin, and it can be applied to a range of toxins.
Abstract
AB toxins consist of an enzymatic A subunit and a cell-binding B subunit1. These toxins are secreted into the extracellular milieu, but they act upon targets within the eukaryotic cytosol. Some AB toxins travel by vesicle carriers from the cell surface to the endoplasmic reticulum (ER) before entering the cytosol2-4. In the ER, the catalytic A chain dissociates from the rest of the toxin and moves through a protein-conducting channel to reach its cytosolic target5. The translocated, cytosolic A chain is difficult to detect because toxin trafficking to the ER is an extremely inefficient process: most internalized toxin is routed to the lysosomes for degradation, so only a small fraction of surface-bound toxin reaches the Golgi apparatus and ER6-12.
To monitor toxin translocation from the ER to the cytosol in cultured cells, we combined a subcellular fractionation protocol with the highly sensitive detection method of surface plasmon resonance (SPR)13-15. The plasma membrane of toxin-treated cells is selectively permeabilized with digitonin, allowing collection of a cytosolic fraction which is subsequently perfused over an SPR sensor coated with an anti-toxin A chain antibody. The antibody-coated sensor can capture and detect pg/mL quantities of cytosolic toxin. With this protocol, it is possible to follow the kinetics of toxin entry into the cytosol and to characterize inhibitory effects on the translocation event. The concentration of cytosolic toxin can also be calculated from a standard curve generated with known quantities of A chain standards that have been perfused over the sensor. Our method represents a rapid, sensitive, and quantitative detection system that does not require radiolabeling or other modifications to the target toxin.
Protocol
1. Preparation of digitonin
- Add 500 μL of 100% ethanol to a microcentrifuge tube and place it in a heat block set at 80 °C for 10 min.
- Dissolve 2.5 mg of digitonin in 250 μL of the heated ethanol to produce a 1% stock solution of digitonin.
- To generate a working solution of 0.04% digitonin, add 40 μL of the digitonin stock solution to 960 μL of HCN buffer (50 mM Hepes pH 7.5, 150 mM NaCl, 2 mM CaCl2, 10 mM N-ethylmaleimide, and a protease inhibitor cocktail).
2. Cell intoxication and permeabilization
Our translocation assay can be applied to a range of toxins and cell lines. Below, we provide a detailed protocol for the detection of cholera toxin (CT). An overview of the procedure is provided in Figure 1.
- HeLa cells are seeded in 6-well plates containing 1 mL DMEM supplemented with 10% fetal bovine serum and antibiotic-antimycotic to achieve 1×106 cells/well after an overnight incubation at 37 °C. To generate enough cytosolic toxin for reproducible detection, triplicate wells are required for each condition.
- Following an overnight incubation, replace the culture medium with 1 mL DMEM containing 100 ng/mL of ganglioside GM1. This increases the number of binding sites for CT, as the GM1 receptor of CT will intercalate into the plasma membrane of cells exposed to a solution of GM1.
- After a 1 hr incubation at 37 °C, remove the GM1-containing medium and wash the cells twice with DMEM. Then, place the cells at 4 °C for 30 min in 1 mL DMEM containing 1 μg/mL of CT.
- Remove the toxin-containing medium, wash the cells twice with DMEM, and incubate the cells in 1 mL DMEM at 37 °C for the desired time interval(s).
- At the end of each chase period, wash the cells with PBS and incubate each well with 250 μL of 0.5 mM EDTA in PBS. Let the cells sit for 10 min at room temperature and then remove them from the 6-well plate by vigorous trituration with a p1000 pipetman. After one well of cells has been collected, combine it with the second and then third well from the same condition. Cell scrapers can also be used to collect the cells.
- Place the combined cell suspension from the three replicate wells (750 μL total volume) in a single microcentrifuge tube, and spin it in a tabletop microcentrifuge for 5 min at 5,000 x g. Cell pellets of roughly equivalent size should be obtained for all conditions.
- Discard the supernatant and resuspend the cell pellet in 100 μL of the 0.04% working solution of digitonin. Place the cell suspension on ice for 10 min.
- Spin the digitonin-permeabilized cells at 16,000 x g for 10 min in a tabletop microcentrifuge. Transfer the cytosol-containing supernatant fraction to a fresh microcentrifuge tube, and retain the organelle-containing pellet fraction.
3. Sample preparation
- Cytosol-containing supernatant fractions are diluted in HCN buffer to a final volume of 1 mL. Sample volumes of at least 1 mL are necessary to ensure air is purged from the 500 μL sample loop before injection.
- Organelle-containing pellet fractions are resuspended in 1 mL of HCN buffer containing 1% Triton X-100. Addition of detergent is necessary to release the membrane-encased pool of toxin.
- Toxin standards at concentrations of 100, 10, 1, and 0.1 ng/mL are prepared in HCN buffer.
- Parallel sets of cytosolic and organelle fractions are prepared for a control experiment to confirm the fidelity of the fractionation procedure. Fractions generated as described in Section 2 are resuspended in 20 μL of 4x sample buffer (cytosolic fraction) or 120 μL of 1x sample buffer (organelle fraction). Equivalent volumes of each fraction are resolved by sodium dodecyl sulfate polyacrylamide gel electrophoresis and probed by Western blot analysis to demonstrate the partitioning of a cytosolic protein in the supernatant fraction and a soluble, resident ER protein in the pellet fraction16-19.
4. SPR slide preparation
- The Reichert SR7000 SPR Refractometer is used for SPR experiments.
- Set a gold-plated glass slide with a self-assembled monolayer in the SPR instrument. To activate the sensor slide, perfuse a 1:1 (v:v) solution of 0.4 M EDC and 0.1 M NHS over the slide for 10 min at a flow rate of 41 μL/min. All subsequent perfusions will use the same flow rate.
- To remove the EDC:NHS activation buffer, wash the plate for 5 min with PBS containing 0.05% Tween 20 (PBST). The plate now contains reactive amide tethers due to uncapping by the EDC:NHS solution.
- Perfuse an anti-CTA antibody over the activated sensor slide at a dilution of 1:20,000 in 20 mM sodium acetate (pH 5.5) for 15 min. An initial drop in the refractive index unit (RIU) will be seen due to the pH change. This will be followed by an increase in the RIU as the antibody is captured by the amide-reactive tethers on the sensor slide.
- Remove unbound antibody from the sensor slide with a 5 minute PBST wash. The RIU signal produced by the captured antibody will plateau and stabilize, providing a new baseline signal.
- Perfuse 1 M ethanolamine (pH 8.5) over the sensor slide for 5 min. This caps and inactivates any unbound tethers left on the sensor slide.
5. SPR analysis of samples
- To establish a baseline reading, perfuse PBST over the antibody-coated sensor for 5 min.
- Perfuse an experimental sample or toxin standard over the sensor for 300 sec. Remove the ligand from the buffer and perfuse PBST over the sensor for another 200 sec.
- Following each perfusion, bound toxin is removed from the sensor by a 100 sec wash with PBST at pH 5.0. This will return the signal to its initial baseline reading, thus allowing another sample to be processed on the same sensor.
- Before loading a new sample, push a small amount of air through the sample loop to expel any residual fluid from the prior sample. Using the procedure outlined in 5.2-5.4, we have run up to 12 samples on one slide without substantial loss of the baseline signal.
- Data analysis is performed with the Scrubber 2 software, and the Igor software is used for figure preparation.
6. Representative Results
Pertussis toxin (PT) is an AB toxin that moves from the cell surface to the ER before its A chain (PTS1) enters the cytosol3, 12. As shown in Figure 2, our SPR-based translocation assay could detect PTS1 in the cytosol of intoxicated CHO cells. No signal was generated from the cytosol of unintoxicated cells, which confirmed the anti-PTS1 antibody did not cross-react with a component of the host cytosol. The cytosolic fraction from cells intoxicated in the presence of brefeldin A (BfA) also failed to produce a positive signal. BfA prevents toxin transport to the ER translocation site6-8, 12, 20-25 and, thus, A chain delivery to the cytosol. At the end of each run, bound toxin is stripped from the sensor slide. This allowed multiple samples to be screened on a single sensor slide and thereby provided a direct comparison between results obtained with different experimental conditions.
CT is another AB-type, ER-translocating toxin4. In Figure 3A, CTA1 was detected in the cytosolic fraction from CT-treated HeLa cells. This emphasized that our methodology works with multiple cell types and can be applied to any toxin for which an anti-A chain antibody is available. No signal was detected when the cytosolic fraction from CT-treated cells was perfused over an SPR sensor coated with an anti-CTB antibody (Fig. 3B), thus demonstrating that the CTA1 subunit but not the cell-binding CTB pentamer enters the cytosol. Figure 3C shows the signal from the organelle fraction is off-scale in comparison to the weaker signal from the cytosolic fraction. This was consistent with the known inefficiency of CT transport to the ER translocation site6, 7, which in turn limits the amount of toxin that can reach the cytosol. Furthermore, the organelle fraction contains CT holotoxin as well as ER-localized CTA1, so the resulting SPR signal for the organelle fraction is inflated by the additional mass of the holotoxin-associated CTB pentamer. Thus, it is not practical to plot data from the organelle and cytosolic fractions on the same sensorgram.
Our assay can monitor the time-dependent accumulation of translocated, cytosolic toxin (Fig 4). Cells were exposed to CT at 4 °C, a temperature that allows toxin binding to the plasma membrane but prevents internalization of the cell-associated toxin. After the removal of unbound toxin, the cells were warmed to 37 °C. Both toxin transport to the ER and A chain translocation to the cytosol can occur at this temperature. No toxin was detected in the cytosol 15 minutes after warming to 37 °C. This reflected the lag time required for (i) holotoxin trafficking to the ER; (ii) A/B subunit dissociation in the ER; and (iii) A chain export to the cytosol. A minor pool of cytosolic toxin was detected after 30 minutes at 37 °C, and progressively larger quantities of cytosolic toxin were detected after the 45 and 60 minute chase intervals. Even greater levels of cytosolic toxin were detected after a 5 hour chase interval17, thus demonstrating a continual, long-term delivery of cell-associated toxin to the host cytosol.
Our assay can also detect the inhibition of toxin translocation to the cytosol (Fig. 5). Cells treated with 10% dimethyl sulfoxide (DMSO), a chemical chaperone that prevents the thermal disordering of the isolated CTA1 subunit (T. Banerjee and K. Teter, unpublished observations), exhibited low levels of cytosolic CTA1 in comparison to the untreated control cells. Unfolding of the toxin A chain is a prerequisite for translocation to the cytosol16-18, so the DMSO-induced stabilization of CTA1 accordingly prevented its movement from the ER to the cytosol.
The association rate constant (ka) calculated from SPR experiments is directly proportional to the concentration of ligand in the perfusion buffer14, 15, 26. Thus, it is possible to determine the concentration of cytosolic toxin from a graph that plots the ka values for toxin standards as a function of toxin concentration. This procedure was used to quantify the DMSO-induced block of toxin translocation presented in Figure 5: the standard curve generated from known concentrations of toxin was used to calculate a cytosolic CTA1 concentration of 0.3 ng/mL for untreated cells and 0.1 ng/mL for DMSO-treated cells (Fig. 6). The inhibition of CTA1 unfolding by DMSO thus generated a 3-fold reduction in the ER-to-cytosol translocation of CTA1.
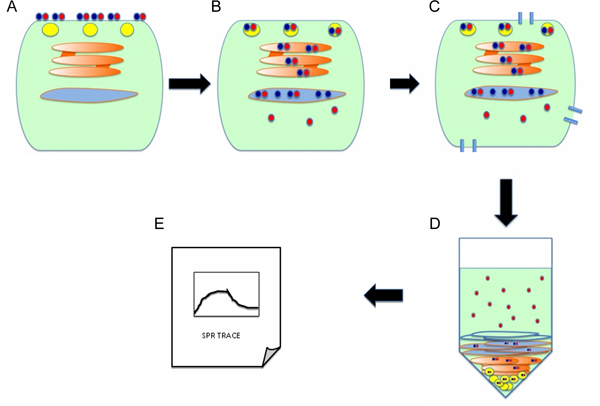
Figure 1. Protocol overview. (A) Cells are incubated with the AB toxin at 4 °C, a temperature that allows toxin binding to the cell surface but prevents toxin endocytosis. The A and B subunits of the toxin are represented by red and blue circles, respectively. (B) Unbound toxin is removed from the medium, and cells are warmed to 37 °C in order to promote endocytosis and retrograde transport of the holotoxin to the ER. Holotoxin dissociation occurs in the ER, which allows the isolated A chain to enter the cytosol by passing through a protein-conducting channel(s) in the ER membrane. (C) Cells are treated with digitonin in order to selectively permeabilize the plasma membrane. (D) Centrifugation is used to partition the cells into separate cytosolic and organelle fractions. The cytosol is squeezed out of the cell through the digitonin-generated pores and is located in the supernatant. The intact, membrane-bound organelles are found in the pellet fraction. (E) To detect the translocated pool of toxin A chain in the host cytosol, the supernatant fraction is perfused over an SPR sensor coated with an anti-A chain antibody.
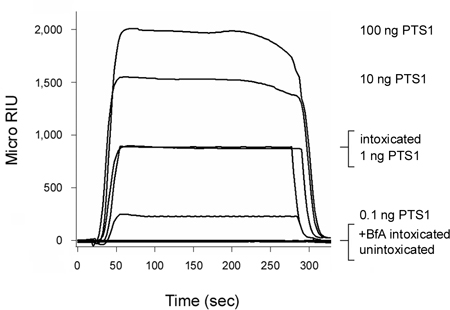
Figure 2. Detection of PTS1 translocation into the host cytosol. CHO cells were pulse-labeled at 4 °C for 30 min with 1 μg/mL of PT. The cells were then chased for 3 hr at 37 °C in toxin-free medium containing no additions (intoxicated) or 5 μg BfA/mL (+BfA intoxicated). Permeabilization of the plasma membrane with digitonin was used to partition cell extracts into separate organelle and cytosolic fractions. An SPR sensor coated with an anti-PTS1 antibody was used to detect the cytosolic pool of PTS1 from untreated or BfA-treated cells. PTS1 standards were perfused over the sensor as positive controls, while the cytosolic fraction from unintoxicated cells was perfused over the sensor slide as a negative control. At the end of each run, bound sample was stripped from the sensor slide.
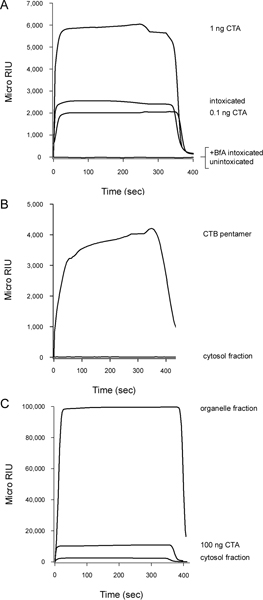
Figure 3. Detection of CTA1 translocation into the host cytosol. HeLa cells pulse-labeled at 4 °C with 1 μg/mL of CT were chased for 2 hr at 37 °C in toxin-free medium containing no additions (intoxicated) or 5 μg BfA/mL (+BfA intoxicated). Permeabilization of the plasma membrane with digitonin was used to partition cell extracts into separate organelle and cytosolic fractions. (A) The cytosolic fractions were perfused over an SPR sensor coated with an anti-CTA antibody. Known quantities of CTA were used as positive controls, while the cytosol from unintoxicated cells was used as a negative control. (B) The cytosolic fraction from cells intoxicated in the absence of BfA was perfused over an SPR sensor coated with an anti-CTB antibody. A purified CTB pentamer was perfused over the slide as a positive control. (C) The organelle fraction was solubilized with 1% Triton X-100 before perfusion over a SPR sensor coated with an anti-CTA antibody. For comparative purposes, the cytosolic fraction (1 mL final volume) from the same cell extract and a CTA standard were also perfused over the sensor. For all panels, bound sample was stripped from the sensor at the end of each run.
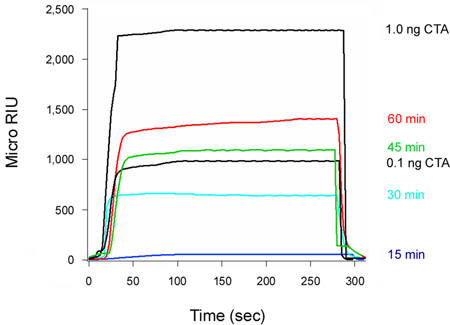
Figure 4. Kinetics of CTA1 entry into the cytosol. HeLa cells pulse-labeled at 4 °C with 1 μg/mL of CT were chased for 15, 30, 45, or 60 min at 37 °C in toxin-free medium. To detect the translocated pool of toxin, cytosolic fractions from digitonin-permeabilized cells were perfused over an SPR sensor coated with an anti-CTA antibody. CTA standards were perfused over the sensor as well. At the end of each run, bound sample was stripped from the sensor slide.
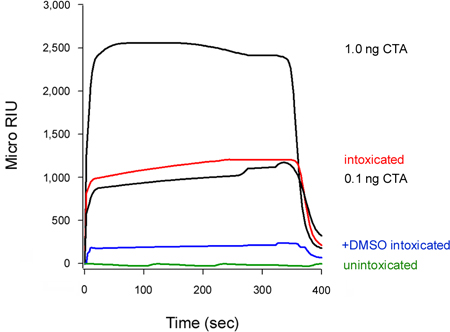
Figure 5. Inhibition of CTA1 translocation by DMSO. HeLa cells pulse-labeled at 4 °C with 1 μg/mL of CT were chased for 2 hr at 37 °C in toxin-free medium containing no additions (intoxicated) or 10% DMSO (+DMSO intoxicated). To detect the translocated pool of toxin, cytosolic fractions from digitonin-permeabilized cells were perfused over an SPR sensor coated with an anti-CTA antibody. CTA standards (100, 10, 1, and 0.1 ng/mL) were perfused over the sensor as positive controls; only the 1 and 0.1 ng/mL standards are shown for scaling purposes. The cytosol from unintoxicated cells was used as a negative control. At the end of each run, bound sample was stripped from the sensor slide.

Figure 6. Calculation of cytosolic CTA1. ka values for the CTA standards from Figure 5 were plotted as a function of toxin concentration. The resulting standard curve was used to determine, based on the ka values of the experimental samples from Figure 5, the concentration of cytosolic CTA1 in untreated and DMSO-treated cells. Toxin standards are presented as filled circles; the untreated cytosol is presented as an open square; and the DMSO-treated cytosol is presented as an open circle. The averages ± ranges of two independent experiments are shown.
Discussion
Comparison to existing methodology
Our SPR-based translocation assay represents a rapid, sensitive, and quantitative method to detect toxin delivery into the host cytosol. The technique does not require radiolabeling or other modifications to the toxin, and it can be applied to any toxin for which an anti-toxin A chain antibody is available. Existing methods to monitor toxin passage into the cytosol also rely upon a subcellular fractionation protocol to partition cell extracts into separate cytosol and membrane fractions11, 23, 27, 28. These methods use Western blot or radiolabels to detect the cytosolic pool of toxin. The former approach is semi-quantitative at best and suffers from relatively poor sensitivity. Even radiolabeling protocols can take weeks to generate a result, owing to the low levels of toxin which reach the cytosol. While quantitative analysis with a radiolabeled toxin can determine the relative percentage of cell-associated toxin which enters the cytosol, this approach cannot directly determine the exact number of cytosolic toxin molecules. Comparing the sensitivity of SPR toxin detection to the detection of radiolabeled toxin is therefore problematic, as the quantity of cytosolic toxin can be calculated by SPR but not by radiolabeling.
Other translocation assays bypass the upstream toxin trafficking steps and deliver the toxin A chain directly to the ER using either plasmid-based expression systems or in vitro transcription / translation systems29-38. For either method, an amino-terminal signal sequence targets the A chain for co-translational import into the ER lumen. Export of the synthesized A chain from the ER is then detected by subcellular fractionation, differential centrifugation, toxin activity in the cytosol, proteasomal degradation of the translocated toxin, and/or a cytosolic-specific toxin modification. Subsets of these approaches focus solely on the translocation event, can be used for in vitro reconstitution experiments, and produce elevated levels of toxin for detection and co-immunoprecipitation studies. However, the methodologies cannot determine the kinetics or efficiency of toxin delivery from the cell surface to the cytosol. It is also possible that the translocated A chain does not enter the ER in the same conformational state as the holotoxin-delivered A chain. Other aspects of host-toxin interactions are missing from these procedures, such as the A/B dissociation event. Thus, there are both strengths and weaknesses to monitoring translocation with A chains that are synthesized directly in the ER.
Toxin translocation is often detected through intoxication assays. The cytotoxic or cytopathic effect generated by exogenously applied toxin demonstrates the toxin A chain has reached its cytosolic target. Obviously, this is an indirect measure of translocation that monitors toxin activity in the cytosol rather than the physical presence of cytosolic toxin. Thus, the technique can neither quantify the levels of cytosolic toxin nor directly detect altered processing of the translocated toxin. There are also scenarios in which a direct correlation between cytosolic toxin levels and toxin activity do not exist, such as the possible need for a threshold concentration of cytosolic toxin to elicit a cellular response or when toxin activity produces a saturated cellular response. Still, intoxication assays can provide a functional correlation to assays which directly document the translocation event. We have previously used this strategy to demonstrate an inhibition of A chain translocation corresponds to an inhibition of cellular intoxication17-19.
In summary, there are multiple methods to detect toxin delivery to the cytosol. Our SPR-based approach has the advantages of providing rapid, sensitive, and quantitative results. The data can also be supplemented with experiments using one of the aforementioned older strategies to generate a stronger conclusion.
Future applications
Our label-free method for the detection and quantification of cytosolic toxin provides investigators with the flexibility to address many outstanding questions regarding the cell biology of intoxication. For example, it is possible to establish the efficiency of A chain delivery to the cytosol by calculating the percentage of surface-bound toxin that reaches the cytosol. It is also possible to quantify the total amount of cytosolic toxin and, by extension, the number of cytosolic toxin molecules per cell. It is believed that one molecule of cytosolic diphtheria toxin is sufficient to elicit a complete cytopathic/cytotoxic effect39; this model can now be tested with other toxins using our translocation assay and correlative intoxication assays. Thus, our SPR-based assay should be able to determine how many molecules of cytosolic toxin are required for productive intoxication. Our technique can also track the persistence of cytosolic toxin. Substantial degradation of the translocated A chain would limit and possibly reduce its cytosolic concentration over time, which would imply the effects of intoxication could be reversed if A chain access to the cytosol was restricted after the initial toxin exposure. Furthermore, the extracellular medium and membrane pellet from intoxicated cells can be used to track the quantity of secreted toxin or toxin residing in the endomembrane system, respectively. Comparative studies of extracellular, endomembrane-localized, and cytosolic toxin can be used to examine how the cell biology of intoxication varies for different ER-translocating toxins. Our assay can also be used to dissect the toxin-specific cellular factors required for the translocation event19. It should be possible to adapt our methodology to track the endosome-to-cytosol translocation of other AB toxins such as anthrax lethal factor and diphtheria toxin. Finally, viral entry into the host cytosol could possibly be monitored with a similar experimental procedure.
Limitations
Conditions that inhibit toxin trafficking to the ER will also prevent toxin delivery to the cytosol. This was demonstrated by the absence of cytosolic toxin in BfA-treated cells (Figs. 2, 3A). Thus, additional control experiments are required when using this method to examine potential blocks of toxin translocation. For some AB toxins, reduction of a disulfide bond that tethers the catalytic subunit to its holotoxin occurs in the ER6, 40-43. The redox status of the A chain can accordingly be used as a measure of toxin transport to the ER16, 18. Recombinant toxins containing the consensus sequence for N-linked glycosylation, a modification that is initiated in the ER, have also been used to detect toxin entry into the ER12, 23, 44-46. Finally, as discussed above, alternative protocols involving co-translational insertion of the toxin A chain into the ER lumen can verify an inhibitory effect on the translocation event. For example, our SPR-based translocation assay demonstrated a functional role for Hsp90 in CTA1 translocation that was confirmed with a plasmid-based system that expressed CTA1 directly in the ER lumen19.
The A chains of ER-translocating toxins exhibit a strong arginine-over-lysine amino acid bias that allows the translocated toxin to evade ubiquitin-dependent proteasomal degradation47-50. However, degradation of the cytosolic toxin still occurs by a relatively slow, ubiquitin-independent proteasomal mechanism51, 52. Conditions that enhance proteasomal activity could thus skew the results of our translocation assay by reducing the pool of translocated toxin in the cytosolic fraction. Cells exposed to a proteasome inhibitor can be used to control for this possibility; an increase in cytosolic toxin resulting from proteasomal inhibition would indicate the toxin could indeed reach the cytosol but was degraded before detection.
It should be noted that these considerations apply to subsets of the aforementioned alternative approaches and are not unique to our method. As mentioned earlier, the best strategy for characterizing the translocation event is to use a combination of well-controlled techniques.
Critical steps and trouble-shooting
Chemical preparation is a critical step for the assay. Digitonin does not dissolve easily, and it should be prepared fresh for every experiment. Likewise, fresh PBST should be used for SPR analysis. The EDC:NHS activation buffer should be prepared immediately before use; it will not retain activity if stored after mixing the two solutions. However, separate aliquots of EDC and NHS can be stored at -80°C and thawed once before use. All solutions, including the samples, should be de-gassed before injection. This will prevent air-induced spikes in the SPR signal.
The cell type to be used for this assay must express enough toxin receptors to allow a detectable pool of toxin A chain to reach the cytosol. In some cases, such as the pre-treatment of HeLa cells with GM1 before CT challenge, additional toxin receptors can be added to the surface of target cells. The cell type must also be susceptible to selective permeabilization of the plasma membrane with digitonin. The protocol described herein is effective with HeLa and CHO cells, but other cell types will require an optimization step using Western blot analysis to monitor the clean separation of organelle and cytosolic fractions. We routinely follow the distributions of protein disulfide isomerase (a soluble ER protein) and Hsp90 (a cytosolic protein) for this purpose16-19. The exclusive partitioning of protein disulfide isomerase into the pellet fraction16-19 also ensures that the organelles collected in the membrane pellet are intact. This is a crucial aspect of our method, as the unintentional rupture of intracellular organelles would introduce error into the system by releasing endomembrane-restricted toxin into the cytosolic fraction. SPR-based experiments can also be used to demonstrate that the cytosolic pool of toxin results from a translocation event rather than from the lysis of intracellular organelles. For example, no toxin was detected in the cytosol of BfA-treated cells (Figs. 2, 3A) or cells exposed to toxin for only 15 minutes (Fig. 4). Likewise, the B subunit of CT was not detected in the cytosolic fraction after a two hour toxin exposure (Fig. 3B). Had our protocol resulted in the permeabilization of internal membranes, we would have detected a cytosolic pool of toxin for each of the aforementioned conditions. Establishing the proper protocol for reproducible, selective permeabilization of the plasma membrane is likely to represent the rate-limiting step for assay implementation. Other options for plasma membrane permeabilization are available, but we found that digitonin treatment provided more consistent results than other methods such as treatment with streptolysin O.
The quality of the antibody will also determine the sensitivity of the assay, which can be established with serial dilutions of a toxin standard. For example, we can reproducibly detect as little as 0.1 ng/mL of either PTS1 or CTA standard (Figs. 2-6). The anti-A chain antibody should not recognize the toxin B subunit, and unintoxicated cells should always be used as a control to ensure the antibody does not cross-react with proteins in the host cell. Preliminary experiments will need to optimize the conditions for stripping bound toxin from the antibody, as this can differ for different anti-toxin antibodies.
When monitoring toxin translocation under altered cellular conditions, the toxin standards and cytosolic fraction from untreated control cells should be supplemented to match the conditions in the experimental sample. For example, CTA standards and the untreated cytosolic fraction from Figure 5 were supplemented with 1% DMSO to match the final drug concentration in the cytosolic fraction from DMSO-treated cells. This eliminates possible differences in the SPR signals that might arise from differences in the chemical composition of the collected fractions. Comparisons between cytosolic and organelle fractions would likewise require the addition of 1% Triton X-100 to the cytosolic fraction and standards, as this detergent is used to release the membrane-encased toxin from the organelle fraction for SPR detection. Preliminary experiments have shown the presence of cytosol does not alter the SPR response to toxin standards, so it is not necessary to supplement the toxin standards with cytosol from unintoxicated cells.
Antibody binding to the sensor slide will not occur if the EDC:NHS activation solution is old or if the slide is inserted into the instrument with the gold side face down. Given the manufacturing process, there will be some plate-to-plate variability which can prevent proper EDC:NHS activation and, thus, antibody capture. If antibody binding to the slide is poor, as indicated by a weakly elevated RIU, a second injection can deposit more of the antibody on the plate. The RIU is an arbitrary unit that varies from one experiment to another depending on how much anti-toxin antibody is deposited on the sensor. However, the on and off rates will remain constant.
It is preferable to use a Refractometer with dual channel perfusion chambers, as one channel can be used for the experimental sample and the other channel can be used for buffer alone in order to correct for possible baseline drift. When using a dual chamber instrument, ensure that the anti-toxin antibody is only added to one of the two channels. Samples will subsequently be run through both channels. With a single channel instrument, the compensation for baseline drift involves collection of buffer alone data from the antibody-coated slide prior to sample injection.
Before the beginning of an SPR experiment, ensure the sensor slide is set tight in the instrument and all fittings are secure. Leaks resulting from these issues will generate air spikes in the collected data. Leaks can also be detected by the absence of waste flow, which should always be present. A sample volume greater than the volume of the injection loop is necessary to avoid air spikes as well – for example, we use 1 mL sample volumes with a 500 μL injection loop. An inappropriate amount of immersion oil on the prism will prevent stabilization of the baseline signal. Other issues relating to operation of the SPR instrument are addressed in the Users Guide and Technical Bulletins provided by Reichert.
開示
The authors have nothing to disclose.
Acknowledgements
This work was funded by NIH grant R01 AI073783 to K. Teter. We thank Dr. Shane Massey for assistance in the development of the subcellular fractionation protocol and Helen Burress for critical reading of the manuscript.
Materials
| Name of the reagent | Company | Catalogue number |
| Digitonin | Sigma | D141 |
| Ethanol | Acros | 61509-0010 |
| DMEM | Invitrogen | 11995065 |
| Fetal Bovine Serum | Atlanta Biologicals | S11550 |
| Ganglioside GM1 | Sigma | G7641 |
| CTA | Sigma | C2398 |
| PTS1 | List | 182 |
| NHS (N-Hydroxysuccinimide) | Pierce | 24500 |
| EDC (1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide) | Thermo Scientific | 22981 |
| Ethanolamine | Sigma | E0135 |
| PBST | Medicago | 09-8903-100 |
| Anti-CTA antibody | Santa Cruz Biotech | sc-80747 |
| Anti-CTB antibody | Calbiochem | 227040 |
| Anti-PTS1 antibody | Santa Cruz Biotech | sc-57639 |
| Refractometer | Reichert | SR7000, SR7000DC |
| SPR sensor slides | Reichert | 13206060 |
| Syringe pump | Cole Palmer | 780200C |
参考文献
- Sandvig, K., van Deurs, B. Membrane traffic exploited by protein toxins. Annu. Rev. Cell Dev. Biol. 18, 1-24 (2002).
- Watson, P., Spooner, R. A. Toxin entry and trafficking in mammalian cells. Adv. Drug Deliv. Rev. 58, 1581-1596 (2006).
- Carbonetti, N. H. Pertussis toxin and adenylate cyclase toxin: key virulence factors of Bordetella pertussis and cell biology tools. Future Microbiol. 5, 455-469 (2010).
- Wernick, N. L. B., Chinnapen, D. J. -. F., Cho, J. A., Lencer, W. I. Cholera toxin: an intracellular journey into the cytosol by way of the endoplasmic reticulum. Toxins. 2, 310-325 (2010).
- Lord, J. M., Roberts, L. M., Lencer, W. I. Entry of protein toxins into mammalian cells by crossing the endoplasmic reticulum membrane: co-opting basic mechanisms of endoplasmic reticulum-associated degradation. Curr. Top. Microbiol. Immunol. 300, 149-168 (2005).
- Lencer, W. I. Entry of cholera toxin into polarized human intestinal epithelial cells. Identification of an early brefeldin A sensitive event required for A1-peptide generation. J. Clin. Invest. 92, 2941-2951 (1993).
- Orlandi, P. A., Curran, P. K., Fishman, P. H. Brefeldin A blocks the response of cultured cells to cholera toxin. Implications for intracellular trafficking in toxin action. J. Biol. Chem. 268, 12010-12016 (1993).
- Sandvig, K., Prydz, K., Hansen, S. H., van Deurs, B. Ricin transport in brefeldin A-treated cells: correlation between Golgi structure and toxic effect. J. Cell. Biol. 115, 971-981 (1991).
- Sandvig, K., Prydz, K., Ryd, M., van Deurs, B. Endocytosis and intracellular transport of the glycolipid-binding ligand Shiga toxin in polarized MDCK cells. J. Cell Biol. 113, 553-562 (1991).
- van Deurs, B. Estimation of the amount of internalized ricin that reaches the trans-Golgi network. J. Cell Biol. 106, 253-267 (1988).
- Tam, P. J., Lingwood, C. A. Membrane cytosolic translocation of verotoxin A1 subunit in target cells. 微生物学. 153, 2700-2710 (2007).
- Plaut, R. D., Carbonetti, N. H. Retrograde transport of pertussis toxin in the mammalian cell. Cell. Microbiol. 10, 1130-1139 (2008).
- Willander, M., Al-Hilli, S. Analysis of biomolecules using surface plasmons. Methods Mol. Biol. 544, 201-229 (2009).
- Homola, J. Present and future of surface plasmon resonance biosensors. Anal. Bioanal. Chem. 377, 528-539 (2003).
- Medaglia, M. V., Fisher, R. J., Golemis, E. . Protein-Protein Interactions. , 255-272 (2002).
- Banerjee, T. Contribution of subdomain structure to the thermal stability of the cholera toxin A1 subunit. 生化学. 49, 8839-8846 (2010).
- Massey, S. Stabilization of the tertiary structure of the cholera toxin A1 subunit inhibits toxin dislocation and cellular intoxication. J. Mol. Biol. 393, 1083-1096 (2009).
- Taylor, M. A therapeutic chemical chaperone inhibits cholera intoxication and unfolding/translocation of the cholera toxin A1 subunit. PLoS ONE. 6, e18825-e18825 (2011).
- Taylor, M. Hsp90 is required for transfer of the cholera toxin A1 subunit from the endoplasmic reticulum to the cytosol. J. Biol. Chem. 285, 31261-31267 (2010).
- Donta, S. T., Beristain, S., Tomicic, T. K. Inhibition of heat-labile cholera and Escherichia coli enterotoxins by brefeldin A. Infect. Immun. 61, 3282-3286 (1993).
- Donta, S. T., Tomicic, T. K., Donohue-Rolfe, A. Inhibition of Shiga-like toxins by brefeldin. A. J. Infect. Dis. 171, 721-724 (1995).
- Nambiar, M. P., Oda, T., Chen, C., Kuwazuru, Y., Wu, H. C. Involvement of the Golgi region in the intracellular trafficking of cholera toxin. J. Cell. Physiol. 154, 222-228 (1993).
- Rapak, A., Falnes, P. O., Olsnes, S. Retrograde transport of mutant ricin to the endoplasmic reticulum with subsequent translocation to cytosol. Proc. Natl. Acad. Sci. U. S. A. 94, 3783-3788 (1997).
- Xu, Y., Barbieri, J. T. Pertussis toxin-mediated ADP-ribosylation of target proteins in Chinese hamster ovary cells involves a vesicle trafficking mechanism. Infect. Immun. 63, 825-832 (1995).
- Yoshida, T., Chen, C. C., Zhang, M. S., Wu, H. C. Disruption of the Golgi apparatus by brefeldin A inhibits the cytotoxicity of ricin, modeccin, and Pseudomonas toxin. Exp. Cell Res. 192, 389-395 (1991).
- Godber, B. Direct quantification of analyte concentration by resonant acoustic profiling. Clin. Chem. 51, 1962-1972 (2005).
- Bernardi, K. M., Forster, M. L., Lencer, W. I., Tsai, B. Derlin-1 facilitates the retro-translocation of cholera toxin. Mol. Biol. Cell. 19, 877-884 (2008).
- Wernick, N. L., De Luca, H., Kam, W. R., Lencer, W. I. N-terminal Extension of the Cholera Toxin A1-chain Causes Rapid Degradation after Retrotranslocation from Endoplasmic Reticulum to Cytosol. J. Biol. Chem. 285, 6145-6152 (2010).
- Simpson, J. C. Ricin A chain utilises the endoplasmic reticulum-associated protein degradation pathway to enter the cytosol of yeast. FEBS. Lett. 459, 80-84 (1999).
- Veithen, A., Raze, D., Locht, C. Intracellular trafficking and membrane translocation of pertussis toxin into host cells. Int. J. Med. Microbiol. 290, 409-413 (2000).
- Castro, M. G., McNamara, U., Carbonetti, N. H. Expression, activity and cytotoxicity of pertussis toxin S1 subunit in transfected mammalian cells. Cell. Microbiol. 3, 45-54 (2001).
- Schmitz, A., Herrgen, H., Winkeler, A., Herzog, V. Cholera toxin is exported from microsomes by the Sec61p complex. J. Cell Biol. 148, 1203-1212 (2000).
- Teter, K., Allyn, R. L., Jobling, M. G., Holmes, R. K. Transfer of the cholera toxin A1 polypeptide from the endoplasmic reticulum to the cytosol is a rapid process facilitated by the endoplasmic reticulum-associated degradation pathway. Infect. Immun. 70, 6166-6171 (2002).
- Winkeler, A., Godderz, D., Herzog, V., Schmitz, A. BiP-dependent export of cholera toxin from endoplasmic reticulum-derived microsomes. FEBS Lett. 554, 439-442 (2003).
- Yu, M., Haslam, D. B. Shiga toxin is transported from the endoplasmic reticulum following interaction with the luminal chaperone HEDJ/ERdj3. Infect. Immun. 73, 2524-2532 (2005).
- LaPointe, P., Wei, X., Gariepy, J. A role for the protease-sensitive loop region of Shiga-like toxin 1 in the retrotranslocation of its A1 domain from the endoplasmic reticulum lumen. J. Biol. Chem. 280, 23310-23318 (2005).
- Teter, K., Jobling, M. G., Sentz, D., Holmes, R. K. The cholera toxin A13 subdomain is essential for interaction with ADP-ribosylation factor 6 and full toxic activity but is not required for translocation from the endoplasmic reticulum to the cytosol. Infect. Immun. 74, 2259-2267 (2006).
- Redmann, V. Dislocation of ricin toxin a chains in human cells utilizes selective cellular factors. J. Biol. Chem. 286, 21231-21238 (2011).
- Yamaizumi, M., Mekada, E., Uchida, T., Okada, Y. One molecule of diphtheria toxin fragment A introduced into a cell can kill the cell. Cell. 15, 245-250 (1978).
- Bellisola, G. Reductive activation of ricin and ricin A-chain immunotoxins by protein disulfide isomerase and thioredoxin reductase. Biochem. Pharmacol. 67, 1721-1731 (2004).
- McKee, M. L., FitzGerald, D. J. Reduction of furin-nicked Pseudomonas exotoxin A: an unfolding story. 生化学. 38, 16507-16513 (1999).
- Orlandi, P. A. Protein-disulfide isomerase-mediated reduction of the A subunit of cholera toxin in a human intestinal cell line. J. Biol. Chem. 272, 4591-4599 (1997).
- Spooner, R. A. Protein disulphide-isomerase reduces ricin to its A and B chains in the endoplasmic reticulum. Biochem. J. 383, 285-293 (2004).
- Fujinaga, Y. Gangliosides that associate with lipid rafts mediate transport of cholera and related toxins from the plasma membrane to endoplasmic reticulm. Mol. Biol. Cell. 14, 4783-4793 (2003).
- Guerra, L. Cellular internalization of cytolethal distending toxin: a new end to a known pathway. Cell. Microbiol. 7, 921-934 (2005).
- Johannes, L., Tenza, D., Antony, C., Goud, B. Retrograde transport of KDEL-bearing B-fragment of Shiga toxin. J. Biol. Chem. 272, 19554-19561 (1997).
- Deeks, E. D. The low lysine content of ricin A chain reduces the risk of proteolytic degradation after translocation from the endoplasmic reticulum to the cytosol. 生化学. 41, 3405-3413 (2002).
- Hazes, B., Read, R. J. Accumulating evidence suggests that several AB-toxins subvert the endoplasmic reticulum-associated protein degradation pathway to enter target cells. 生化学. 36, 11051-11054 (1997).
- Rodighiero, C., Tsai, B., Rapoport, T. A., Lencer, W. I. Role of ubiquitination in retro-translocation of cholera toxin and escape of cytosolic degradation. EMBO Rep. 3, 1222-1227 (2002).
- Worthington, Z. E., Carbonetti, N. H. Evading the proteasome: absence of lysine residues contributes to pertussis toxin activity by evasion of proteasome degradation. Infect. Immun. 75, 2946-2953 (2007).
- Pande, A. H., Moe, D., Jamnadas, M., Tatulian, S. A., Teter, K. The pertussis toxin S1 subunit is a thermally unstable protein susceptible to degradation by the 20S proteasome. 生化学. 45, 13734-13740 (2006).
- Pande, A. H. Conformational instability of the cholera toxin A1 polypeptide. J. Mol. Biol. 374, 1114-1128 (2007).

