Modified Spared Nerve Injury Surgery Model of Neuropathic Pain in Mice
Summary
The modified surgery is a simplified method for mouse or rat spared nerve injury model that requires only one ligation and one cut to injure both common peroneal and sural nerves.
Abstract
Spared nerve injury (SNI) is an animal model that mimics the cardinal symptoms of peripheral nerve injury for studying the molecular and cellular mechanism of neuropathic pain in mice and rats. Currently, there are two types of SNI model, one to cut and ligate the common peroneal and the tibial nerves with intact sural nerve, which is defined as SNIs in this study, and another to cut and ligate the common peroneal and the sural nerves with intact tibial nerve, which is defined as SNIt in this study. Because the sural nerve is purely sensory whereas the tibial nerve contains both motor and sensory fibers, the SNIt model has much less motor deficit than the SNIs model. In the traditional SNIt mouse model, the common peroneal and the sural nerves are cut and ligated separately. Here a modified SNIt surgery method is described to damage both common peroneal and sural nerves with only one ligation and one cut with a shorter procedure time, which is easier to perform and reduces the potential risk of stretching the sciatic or tibial nerves, and produces similar mechanical hypersensitivity as the traditional SNIt model.
Introduction
Nerve injury-induced neuropathic pain following surgery or trauma has a significant economic burden that impairs quality of life. A host of nerve injury models, including spinal nerve ligation (SNL)1, chronic constriction injury (CCI)2 to the sciatic nerve, partial sciatic nerve ligation (pSNL)3, sciatic nerve transaction (SNT)4 and spared nerve injury (SNI)5,6,7,8, were successfully developed to mimic the cardinal symptoms of peripheral nerve injury in rats and mice for studying the molecular and cellular mechanism of neuropathic pain6,7,8,9,10. However, each surgical model has its benefits and limitations, therefore particular attention should be given to exploring and developing the surgery models10.
The rodent SNI model produces long-term hypersensitivity to mechanical stimulation. However, it is somewhat confusing because there are two different SNI models. The initial SNI model was developed in Woolf's lab, in which the common peroneal and the tibial nerves were injured, leaving the sural nerve intact5,6. The second SNI model was developed in Basbaum's lab, in which the common peroneal and the sural nerves were injured, leaving the tibial nerve intact7,8. The initial Woolf's model is defined as SNIs here because the sural nerve is left intact, and Basbaum's model is defined as SNIt here because the tibial nerve is left intact. Because the sural nerve is purely sensory whereas the tibial nerve contains both motor and sensory fibers, the SNIt model has much less motor deficit than the SNIs model. However, unlike the SNIs model, mice in the SNIt model do not develop thermal hypersensitivity, but mechanical hypersensitivity develops in both models. Although the SNIt model is a relatively easy procedure, it requires the ligation of the sural and common peroneal nerves separately with the potential risk of stretching the sciatic or tibial nerves6,7,8,9.
The common peroneal, tibial, and sural nerves are three branches of the sciatic nerve and can be clearly identified at the superior edge of the gastrocnemius muscle (Figure 1): the tibial nerve goes under the gastrocnemius muscle, and the common peroneal (cephalad side) and sural nerve (caudal side) are above the gastrocnemius muscle11. Based on its anatomical features, a modified mouse SNIt surgery procedure was developed to ligate the common peroneal and sural nerves together with only one nerve-ligation and one nerve-cutting, which results in shortened procedure-time.
Protocol
Animal experiments were approved by UCSF Institutional Animal Care and Use Committee and were conducted in accordance with the NIH Guide for the Care and Use of Laboratory animals. Adult C57BL/6 mice weighing 20-30 g was used in this study. The von Frey assessment was performed between 1:00 pm and 3:00 pm.
1. Anesthesia and mouse preparation
- Place a mouse in a plastic chamber filled with 2% isoflurane in O2 at a flow rate of 1.0 L/min until it is fully anesthetized.
- Cover the eyes with ophthalmic ointment using a cotton-wool applicator.
- Place the snout of the mouse into a flexible nose cone with 2% isoflurane flow throughout the surgical procedure.
- Place the mouse in a right lateral position. Keep the left leg up with knee flexion and secure it with adhesive tape.
- Remove the hair around the thigh and knee area with an electric shaver and hair removal cream. Disinfect the skin with 2% chlorhexidine and 70% alcohol.
- Ensure sufficient anesthesia depth before surgery by testing no response to pinch stimulus on the hind limb or tail with tweezers as the standard. Provide thermal support to the mouse.
NOTE: No local anesthetic or NSAID was used before and after performing the SNIt model because local anesthetic and NSAID significantly reduce the neuropathic pain behavior after SNIt12.
2. Modified SNIt surgery
- Cut a 1 cm incision starting at the first 1/3 of the horizontal line crossing the knee with an approximately 30° angle from the vertical line with a scalpel (Figure 2A).
- Two white lines can be visualized under the biceps femoris muscle (BFM) after separating skin incision, with the medial (cephalad) thick line as the femur and lateral (caudal) thin line as sciatic nerve (Figure 2B).
- Blunt dissect BFM along the caudal white line with curved micro forceps and micro scissors to expose the sciatic nerve. Avoid blood vessel damage during blunt dissection. If accidental vessel damage occurs, use sterile cotton-wool swabs to absorb blood and apply proper pressure to stop bleeding.
- Differentiate the three branches from the sciatic nerve at the superior edge of the gastrocnemius muscle. The tibial nerve is the one with the biggest diameter passing under the gastrocnemius muscle, whereas the sural nerves (lateral, the smallest diameter) and the common peroneal nerve (medial) run above the gastrocnemius muscle (Figure 2C and Figure 3A).
- Depending on how BFM is dissected and opened, visualize the common peroneal nerve as lateral (Figure 2C) or medial (Figure 3A) to the tibial nerve.
- Separate the common peroneal and the sural nerves from the neighboring tissues using curve micro forceps.
- Ligate the common peroneal and sural nerves together with a 6-0 suture, as both nerves run above the gastrocnemius muscle, but the tibial nerve passes under the gastrocnemius muscle (Figure 2D and Figure 3B,C). Observe the limb for contraction following the tight ligature. For the traditional method, ligate the common peroneal and sural nerves separately.
- Cut nerve at a distal part within 2-4 mm of the ligation with a pair of micro scissors. Ensure that the tibial nerve remains untouched during the whole procedure. For the traditional method, cut the common peroneal and sural nerves at the distal part within 2-4 mm of the ligation and remove a 2 mm section, separately.
- Close the muscular layer with a 6-0 silk suture and the skin incision with wound clips.
- After surgery, return the mice to the animal room until full recovery from anesthesia. Check daily for intact incisions, normal food intake, water consumption, general body condition, regular movements, and grooming. Remove wound clips 7-14 days after surgery.
3. von Frey assessment for mechanical threshold
- Acclimatize the mice for 6 days to the testing room environment and testing materials to perform the von-Frey assessment. Place the mice in clear plastic cylinders on an elevated wire mesh grid for 1 h of habituation. Place white papers between each cylinder to prevent any visual cue from each testing animal.
- During this period, perform habituation every 2 days, and measure the baseline of von Frey monofilaments under the mid-plantar of the hind paw after the last habituation.
- Perform von Frey assessment with a blind tester. Stimulate the mid-plantar of the hind paw with von Frey filaments by using the up-down paradigm13. Apply the von Frey filament to the plantar surface perpendicularly with applied force to cause slight curling.
- Verify positive responses as sudden paw withdrawal, sudden flinching, or sudden paw licking. Exert the next stimulus at an interval of 5 s to avoid the influence of the previous stimulus.
- Confirm mechanical threshold per paw by taking an average of 3 sessions.
- Based on the 50% hind paw withdrawal threshold decided by the up-down method, use the percent response method with 0.16 g filament to assess the difference further.
- Record the percentage of the positive responses after 10 stimuli of 0.16 g filament applied to the mid-plantar of the hind paw regardless of the responses.
- Perform the von Frey assessments on pre-surgery day 1, and post-surgery on days 1, 3, 5, 7, and 14.
4. Statistical Analysis
- Report normally distributed continuous data as mean ± standard error of the mean (SEM). Analyze the continuous data with 2-tailed t-test or two-way repeated-measures ANOVA. Process all data using statistical analysis software, with statistical significance at the level of p < 0.05.
Representative Results
The comparison of procedure time between modified and traditional methods.
The procedure time from the beginning of cutting the skin to the end of closing skin was recorded in 5 mice with the modified approach and 5 mice with the traditional approach, respectively. A minimal number of animals was used to obtain results with statistical significance. Compared with the control of the traditional approach7,14 to perform SNIt, the modified approach took almost half the amount of procedure time (236.2 ± 28.6 s vs. 422.6 ± 53.8 s, p=0.0156; Figure 4).
The comparison of mechanical hypersensitivity between the two methods.
No difference of von Frey assessment (manual) was observed in the two groups at baseline (1.05 ± 0.10 g vs. 0.96 ± 0.13 g, p=0.9405). Compared with the traditional method (n=9), the modified method (n=14) induced similar mechanical hypersensitivity on the ipsilateral side from post-operative day 1 to post-operative day 14 (0.33 ± 0.09 g vs. 0.32 ± 0.05 g, p>0.9999, at post-operative day 1; 0.19 ± 0.02 g vs. 0.27 ± 0.06 g, p=0.9485 , at post-operative day 3; 0.20 ± 0.06 g vs. 0.15 ± 0.05 g, p=0.9979, at post-operative day 5; 0.13 ± 0.02 g vs. 0.15 ± 0.03 g, p>0.9999, at post-operative day 7; and 0.14 ± 0.02 g vs. 0.19 ± 0.03 g, p=0.9937, at post-operative day 14; Figure 5A).
Compared with percentage response between traditional (n=5) and modified method (n=5), similar mechanical hypersensitivity was observed on the ipsilateral side from baseline (4.00% ± 2.45% vs. 6.00% ± 2.45%, p>0.9999) to post-operative day 1 (20.00% ± 3.16% vs. 12.00% ± 3.74%, p=0.8987), day 3 (30.00% ± 5.48% vs. 32.00% ± 4.90%, p>0.9999), day 5 (36.00% ± 9.27% vs. 30.00% ± 5.48%, p=0.9730), day 7 (32.00% ± 8.00% vs. 36.00% ± 4.00%, p=0.9968), and day 14 (38.00% ± 5.83% vs. 36.00% ± 7.48%, p>0.9999; Figure 5B).
No neural reconnection between the distal and remaining stump at post-operative day 14.
Because the axon regeneration proceeds at a rate of 1-3 mm/d15, whether there is nerve regeneration at post-operative day 14 should be taken into account. On the post-operative day 14, the modified SNI mice were perfused intracardially with 0.1 mol/L phosphate-buffered saline followed by a phosphate-buffered 10% formalin fixative, and the nerve ligation site was dissected and exposed. No neural reconnection was observed between the distal and remaining stumps (Figure 3D).

Figure 1. Illustration of the 3 branches of the sciatic nerve that are separated at the superior edge of the gastrocnemius muscle (GM) around the knee area. The tibial nerve runs under the GM muscle, and the common peroneal nerve and sural nerve run above the GM muscle. 1: sciatic nerve; 2: tibial nerve; 3: common peroneal nerve; 4: sural nerve. Abbreviations: BFM = biceps femoris muscle; GM = gastrocnemius muscle. Please click here to view a larger version of this figure.
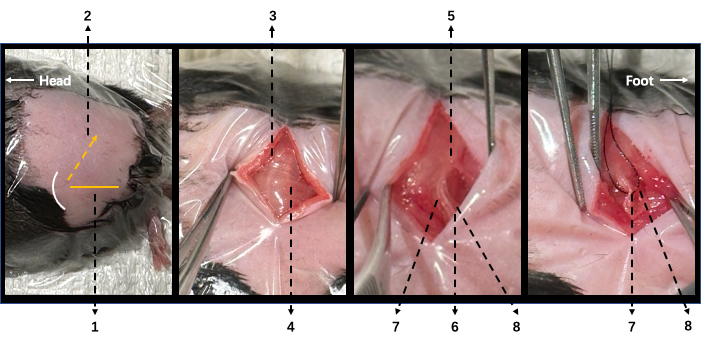
Figure 2. Illustration of surgical procedure in modified SNI mice. (A) In a lateral position, the left leg is upside with knee flexion. The yellow horizontal line (1) indicates the horizontal line crossing the knee level, and the yellow dashed arrow (2) indicates the incision. (B) Following a skin incision, two white lines can be visualized under the biceps femoris muscle (BFM). The femur is under the cephalad one (3), and the sciatic nerve is under the caudal one (4). (C) After careful dissection of BFM, the sciatic nerve (5) and its three branches can be visualized: the tibial (6), common peroneal (7), and sural (8) nerves. (D) The common peroneal (7) and sural (8) nerves were ligated together. 1: horizontal line crossing knee; 2: cut incision; 3: femur on the underneath; 4: sciatic nerve on the underneath; 5: sciatic nerve; 6: tibial nerve; 7: common peroneal nerve; 8: sural nerve; 9: white curve line indicates knee. Please click here to view a larger version of this figure.

Figure 3. Illustration of sciatic, tibial, sural, and common peroneal nerves with the ligation of modified SNI in intracardially perfused mice. (A) Sciatic nerve (1) and its three branches: the tibial nerve (2) passing under the gastrocnemius muscle (5), and the common peroneal (3) and the sural (4) nerves running above the gastrocnemius muscle. (B) Suture needle crossing under common peroneal and sural nerves together. (C) A 6-0 nylon suture was used for the ligation of common peroneal and sural nerves together. (D) No reconnection between distal and remaining nerve stump at post-operative day 14 was observed. 1: sciatic nerve; 2: common peroneal nerve 3: tibial nerve; 4: sural nerve; 5: gastrocnemius muscle; 6: ligation. Please click here to view a larger version of this figure.

Figure 4. The modified method is faster than the traditional SNI method to perform. Compared to the traditional SNI method (n=5), the modified method (n=5) requires much less procedure time to perform. Analyses were performed using an unpaired t-test, and data are presented as mean ± SEM. Please click here to view a larger version of this figure.

Figure 5. von Frey assessment of mechanical responsiveness in traditional and modified SNI models. (A) The modified SNI (n=9) and traditional SNI (n=14) models induced similar mechanical hypersensitivity on the ipsilateral side in 14-day follow-up. (B) The modified SNI (n=5) and traditional SNI (n=5) models acquired similar percentage responses on the ipsilateral side in a 14-day follow-up. Analyses were performed using two-way ANOVA with Sidak's multiple comparisons test. Data are presented as mean ± SEM. Please click here to view a larger version of this figure.
Discussion
Compared to the traditional mouse SNIt method that ligates the common peroneal nerve and the sural nerve separately6,7,8,9, the modified SNIt model has three advantages: (1) it has less risk of contracting or stretching sciatic or tibial nerves; (2) there is no need to remove the distal nerve stumps after nerve-cutting because by ligating the common peroneal nerve and the sural nerve together, the distal nerve stumps are anatomically separated from the proximal stumps. Indeed, anatomy dissection demonstrated that no nerve regeneration was observed 14 days after modified SNIt; (3) the procedure is much easier to perform with a much shorter procedure time.
It is critical to make skin incisions low around knee level, rather than high in the thigh near the hip, when performing the modified mouse SNIt. This is because the common peroneal, tibial, and sural nerves have not branched out from the sciatic nerve at the high thigh area, which makes it challenging to separate the three branches. In contrast, at the superior edge of the gastrocnemius muscle near the knee area, the three branches from the sciatic nerve traverse separately and are easily visualized and identified, as the tibial nerve passing under the gastrocnemius muscle, and the common peroneal nerve on the cranial side and sural nerve on the caudal side running above the gastrocnemius muscle11. Interestingly, although the common peroneal nerve is medial to the tibial nerve at the thigh area, it usually crosses the tibial nerve to get closer to the sural nerve at the superior edge of the gastrocnemius muscle at the knee area in the lateral position with knee flexion, which makes it easier for ligating common peroneal and sural nerves together. Importantly, the tibial nerve remains intact without contacting or stretching when the common peroneal and sural nerves are ligated above the gastrocnemius muscle. In addition, when dissecting BFM to expose underneath nerves, it is important to avoid damaging blood vessels (lateral proximal genicular artery, popliteal artery, distal caudal femoral artery, etc.) located above the gastrocnemius muscle16.
Although this modified SNIt model successfully develops neuropathic pain, some limitations are needed to be admitted. Because of damage to the common peroneal nerve, this could produce motor dysfunction with markedly extended hind leg17. Another, the mechanical hypersensitive area is innervated by intact nerve rather than injured nerve, but the neuropathic pain is often caused by the lesion or disease of the peripheral or central nervous system in clinical pain management18. Therefore, further study needs to be explored in the development of the neuropathic pain model.
In summary, this modified mouse SNIt method is a simplified SNI procedure with only one nerve-ligation and one nerve-cutting without any removal of nerve stumps. It is much easier to perform in producing nerve injury-induced mechanical hypersensitive, with reduced risk of sciatic or tibial nerves damage.
Divulgations
The authors have nothing to disclose.
Acknowledgements
Z.G. is supported by NINDS R01NS100801.
Materials
| 6-0 suture | Henry Schein | 9007482 | Nerve ligation and close the muscular layer |
| Iris Scissors | Integra Miltex | 12460598 | Cut muscle and fascia |
| Mayo dissecting scissors | Fisherbrand | 895120 | Cut skin incision |
| Micro forcep | Fisherbrand | 16100110 | Blunt dissection biceps femoris muscle |
| Micro Scissors | Excelta | 17467496 | Cut nerve |
| Microdissection Forceps | Fisherbrand | 16100123 | Separate the common peroneal and the sural nerves from the neighboring tissues |
| Needle Holder | Fisherbrand | 8966 | Hold 6-0 needle |
| Prism software | Graph Pad | version 8.0 | Statistical analysis software |
| Wound clips | Roboz Surgical | NC1878744 | Close skin incision |
References
- Chung, J. M., Kim, H. K., Chung, K. Segmental spinal nerve ligation model of neuropathic pain. Methods in Molecular Medicine. 99, 35-45 (2004).
- Vissers, K., Adriaensen, H., De Coster, R., De Deyne, C., Meert, T. F. A chronic-constriction injury of the sciatic nerve reduces bilaterally the responsiveness to formalin in rats: a behavioral and hormonal evaluation. Anesthesia and Analgesia. 97 (2), 520-525 (2003).
- Malmberg, A. B., Basbaum, A. I. Partial sciatic nerve injury in the mouse as a model of neuropathic pain: behavioral and neuroanatomical correlates. Pain. 76 (1-2), 215-222 (1998).
- Moore, K. A., et al. Partial peripheral nerve injury promotes a selective loss of GABAergic inhibition in the superficial dorsal horn of the spinal cord. The Journal of Neuroscience: the official journal of the Society for Neuroscience. 22 (15), 6724-6731 (2002).
- Decosterd, I., Woolf, C. J. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 87 (2), 149-158 (2000).
- Cichon, J., Sun, L., Yang, G. Spared Nerve Injury Model of Neuropathic Pain in Mice. Bio-Protocol. 8 (6), 2777 (2018).
- Shields, S. D., Eckert, W. A., Basbaum, A. I. Spared nerve injury model of neuropathic pain in the mouse: a behavioral and anatomic analysis. The Journal of Pain. 4 (8), 465-470 (2003).
- Guan, Z., et al. Injured sensory neuron-derived CSF1 induces microglial proliferation and DAP12-dependent pain. Nature Neuroscience. 19 (1), 94-101 (2016).
- Richner, M., Bjerrum, O. J., Nykjaer, A., Vaegter, C. B. The spared nerve injury (SNI) model of induced mechanical allodynia in mice. Journal of Visualized Experiments: JoVE. (54), e3092 (2011).
- Challa, S. R. Surgical animal models of neuropathic pain: Pros and Cons. The International Journal of Neuroscience. 125 (3), 170-174 (2015).
- Kosaka, Y., et al. Development and persistence of neuropathic pain through microglial activation and KCC2 decreasing after mouse tibial nerve injury. Brain Research. 1733, 146718 (2020).
- Parisien, M., Lima, L. V., Dagostino, C., El-Hachem, N., Drury, G. L., Grant, A. V., Huising, J., Verma, V., Meloto, C. B., Silva, J. R., Dutra, G. C. S., Markova, T., Dang, H., Tessier, P. A., Slade, G. D., Nackley, A. G., Ghasemlou, N., Mogil, J. S., Allegri, M., Diatchenko, L. Acute inflammatory response via neutrophil activation protects against the development of chronic pain. Sci Transl Med. 14 (644), eabj9954 (2022).
- Chaplan, S. R., Bach, F. W., Pogrel, J. W., Chung, J. M., Yaksh, T. L. Quantitative assessment of tactile allodynia in the rat paw. Journal of Neuroscience Methods. 53 (1), 55-63 (1994).
- Bourquin, A. F., et al. Assessment and analysis of mechanical allodynia-like behavior induced by spared nerve injury (SNI) in the mouse. Pain. 122 (1-2), 1-14 (2006).
- Sulaiman, W., Gordon, T. Neurobiology of peripheral nerve injury, regeneration, and functional recovery: from bench top research to bedside application. The Ochsner Journal. 13 (1), 100-108 (2013).
- Kochi, T., et al. Characterization of the arterial anatomy of the murine hindlimb: functional role in the design and understanding of ischemia models. PLoS One. 8 (12), 84047 (2013).
- Omori, Y., et al. A mouse model of sural nerve injury-induced neuropathy: gabapentin inhibits pain-related behaviors and the hyperactivity of wide-dynamic range neurons in the dorsal horn. Journal of Pharmacological Sciences. 109 (4), 532-539 (2009).
- Colloca, L., et al. Neuropathic pain. Nature Reviews. Disease Primers. 3, 17002 (2017).

