Visualizing Field Data Collection Procedures of Exposure and Biomarker Assessments for the Household Air Pollution Intervention Network Trial in India
Summary
We detail the consistent, high-quality procedures used throughout air and biological sampling processes at Indian field sites during a large randomized controlled trial. Insights gathered from the oversight of applications of innovative technologies, adapted for exposure assessment in rural regions, enable better field data collection practices with more reliable outcomes.
Abstract
Here, we present a visual representation of standard procedures to collect population-level data on personal exposures to household air pollution (HAP) from two different study sites in a resource-constrained setting of Tamil Nadu, India. Particulate matter PM2.5 (particles smaller than 2.5 microns in aerodynamic diameter), carbon monoxide (CO), and black carbon (BC) were measured in pregnant mothers (M), other adult women (OAW), and children (C) at various times over a 4 year period. In addition, stove usage monitoring (SUMs) with data-logging thermometers and ambient measurements of air pollution were carried out. Furthermore, the feasibility of collecting biological samples (urine and dried blood spots [DBSs]) from study participants at the field sites was successfully demonstrated. Based on findings from this and earlier studies, the methods used here have enhanced the data quality and avoided issues with household air pollution and biological sample collection in resource-constrained situations. The procedures established may be a valuable educational tool and resource for researchers conducting similar air pollution and health studies in India and other low- and middle-income countries (LMICs).
Introduction
Globally, exposure to household air pollution (HAP), mostly from solid-fuel cooking, is a major cause of morbidity and mortality1,2,3. Cooking and heating with solid fuels (biomass-such as wood, dung, crop residues, and coal) is widespread in low- and middle-income countries (LMICs), posing various health, environmental, and economic issues. PM2.5 is a 'silent killer,' occurring both indoors and outdoors4,5. Indoor air quality in India is often considerably worse than outside air quality, and it has gained enough attention to be regarded as a major environmental health hazard4. A paucity of measurement-based quantitative exposure data has impeded global burden of disease (GBD) evaluations connected with HAP6,7.
Current research often ignores that the measurement of HAP exposures is complicated and varies depending on many factors, including fuel type, stove type, and a mixed use of many clean and unclean stoves, a phenomenon known as "stove stacking". Other influences on exposure include the quantity of fuel consumed, kitchen ventilation levels, the length of time spent in proximity to the cookstove, age, and gender8. The most widely measured and arguably the best indicator of exposure to HAP is PM2.5; however, due to a lack of affordable, user-friendly, and reliable instrumentation, measuring fine particulate matter (PM2.5) has been particularly difficult.
Various studies have reported measuring the level of either single or multiple air pollutants using different methods8,9,10,11,12. In recent years, relatively low-cost sensors that are able to measure these pollutants in indoor and ambient environments have been emerging. However, not all of these sensors are viable for fieldwork for various reasons, including maintenance costs, deployment challenges, issues of comparability with conventional measurement methods, limited human resources to validate these sensors against reference methods, the difficulty of regular data quality checks (through the cloud), and limited or no decentralized troubleshooting facilities. Many of the studies with these types of measurements have used them as a proxy for exposure or by combining environmental measurements with exposure reconstruction using time activity assessments8,9,12,13,14.
Personal monitoring-in which a monitor is carried on or by an individual through space and time-may better capture their 'true' total exposure. Studies that measure personal exposure often only briefly communicate their exact protocols, often in supplementary materials to scientific manuscripts9,12,13,14,15. Although the techniques detailed in these studies provide a solid general sense of sampling methodology, there is often an absence of the specifics of the field data collection stages12,16.
Numerous additional characteristics, in addition to pollutant concentrations, may be monitored in these residences. Stove use monitoring, a method of assessing the time and intensity of use of household energy appliances, is a major part of many recent impact and exposure assessments16,17,18,19. Many of these monitors focus on measuring the temperature at or near the point of combustion on cooking stoves. While thermocouples and thermistors are employed, there is a lack of operating protocols for the monitors, including how best to put them on cookstoves to capture variability in stove usage patterns.
Biomonitoring, similarly, is an effective tool for evaluating environmental exposures, though several factors influence the choice of an optimum biologic matrix20. Under ideal circumstances, sample collection must be non- or minimally invasive. The methods employed should ensure ease of handling, non-restrictive shipping and storage, a good match between the proposed biomarker and biological matrix, a relatively low cost, and no ethical concerns.
Urine sample collection has some major advantages for biomonitoring. As with other sample collection techniques, a range of potential methods exist. Collecting 24 hour void urine can be cumbersome for participants, leading to non-adherence of sample collection20,21. In such cases, spot samples, first morning voids, or other 'convenient' samplings are recommended. The volume of urine collected can be a major disadvantage when collecting spot samples, leading to variability in the concentrations of endogenous and exogenous chemicals. In this case, adjustment using urine creatinine concentrations is a commonly used method for dilution corrections22.
Another commonly collected biospecimen is venous blood. Venous blood samples are often difficult to obtain for biomonitoring; they are intrusive, fear-inducing, and require proper sample handling, storage, and transport. An alternative approach using dried blood spots (DBSs) can be useful for collecting samples in adults and children for biomonitoring23.
A substantial literature gap exists between the simple description of field methods and the publication of detailed, replicable instructions on monitor use and deployment that reflects the true complexity of field data collection of quality-assured samples24,25. Some studies have outlined standard operating procedures (SOP) for measuring air pollutants (indoor and ambient) and monitoring stove use.
However, the essential steps behind the field measurement, laboratory support, and transport of monitoring instruments and samples are very rarely described8,11,25. The challenges and limitations of field-based monitoring in both high- and low-resource settings may be properly captured through video, which could complement written operating procedures and provide a more direct method of showing how devices and sampling and analytical techniques are performed.
In the Household Air Pollution Intervention Network (HAPIN) randomized controlled trial, we used video and written protocols to describe the procedures for measuring three pollutants (PM2.5, CO, and BC), for stove use monitoring and for biospecimen collection. HAPIN involves using harmonized protocols that require strict adherence to SOPs to maximize data quality from samples collected across multiple time points at four study sites (in Peru, Rwanda, Guatemala, and India).
The criteria for study design, site selection, and recruitment are described earlier24,26. The HAPIN trial was conducted in four countries; Clasen et al. described the study settings in detail26. Each study site recruited 800 households (400 intervention and 400 control) with pregnant women between the ages of 18 and 35, who are 9 to 20 weeks gestation, use biomass for cooking at home, and are nonsmokers. In a subset of these households (~120 per country), other adult women were also enrolled in this study.
After recruitment, a total of eight visits were made. The first, at baseline (BL), occurred prior to randomization. The next seven were split up by before birth (at 24-28 weeks gestation [P1], 32-36 weeks gestation [P2]), at birth (B0), and after birth (3 months [B1], 6 months [B2], 9 months [B3], and 12 months [B4]). For M, there were three assessments (BL, P1, and P2), for OAWs, six assessments (BL, P1, P2, B1, B2, and B4), and for C, four assessments (B0, B1, B2, and B4) were performed. At B0, biomarker and health assessments were carried out, while only health assessments were carried out at the B3 visit.
All four countries followed identical protocols. In this manuscript, we describe steps followed in India. The study was performed at two locations in Tamil Nadu: Kallakurichi (KK) and Nagapattinam (NP). These sites are located between 250 and 500 kilometers from the core research facility at the Department of Environmental Health Engineering at Sri Ramachandra Institute of Higher Education and Research (SRIHER) in Chennai, India. The complexity of field data collection protocols requires the deployment of many personnel with varying levels of skills and backgrounds.
We present a written and visual depiction of the steps involved in estimating micro-environmental and personal exposure samples in pregnant mothers (M), other/older adult women (OAW), and children (C) to fine particulate matter, carbon monoxide (CO), and black carbon (BC). Field protocols for (1) monitoring ambient air quality with reference-grade monitors and low-cost sensors, (2) long-term stove use monitoring on conventional and liquefied petroleum gas stoves, and (3) biological sample collection (urine and DBSs) for biomonitoring are also presented. This includes methods for transporting, storing, and archiving environmental and biological samples.
Protocol
The Institutional Ethics Committee at Sri Ramachandra Institute of Higher Education and Research (IEC-N1/16/JUL/54/49), Emory University Institutional Review Board (00089799), and the Indian Council of Medical Research-Health Ministry Screening Committee (5/8/4-30/(Env)/ Indo-US/2016-NCD-I) approved the HAPIN trial. The HAPIN trial is identified as NCT02944682 on clinicaltrials.gov. Written informed consents were collected from the study participants prior to their participation and the study was conducted according to ethical guidelines.
NOTE: The case report forms (CRF) administered during the sampling and data collection are available in the RedCap database, stored at Emory University, and are maintained with the data-sharing agreement between all the collaborators, which can be provided to the readers upon request.
1. Instruments and materials
- Use the following instruments for air pollution monitoring: a microbalance for filter weighing, for microenvironment/personal sampling-Enhanced Children's MicroPEM (ECM) for PM2.5, an optical transmissometer for black carbon (BC) measurement, data loggers for CO and Bluetooth-based beacon, beacon loggers for indirect measurement of PM2.5 (during each visit-BL, P1, P2, B1, B2, and B4), a combined gravimetric and nephelometric monitor for ambient PM2.5 measurements, and temperature loggers for monitoring stove usage.
- Use the following instruments for biomonitoring: cooler and vaccine bags for shipping biospecimens, protein saver cards, humidity indicator cards, an adult lancet, an infant safety lancet, and capillary tubes (40 µL).
2. Filter conditioning and weighing
- Use clean, powder-free gloves to handle the filters. Check the filters (2 µm pore size, 15 and 47 mm diameter) for any damages using a lightbox and place the checked filters in a cleaned filter keeper in an air conditioned room (19-23 °C and 35%-45% relative humidity [RH]) for 24 h.
- Place a clean piece of foil on the desk and switch on the microbalance. Set the scale unit to milligrams (0.001 mg) and follow the internal calibration.
- Record the date/time, technician name, RH, temperature, filter lot number, filter size, and filter ID in the data entry sheet.
- Take the conditioned filter and deionize for 10s. Place the filter carefully on the weighing tray and record the weight as "Weight 1" in the CRF (Supplementary Figure 1).
- Remove the filter, place it in a Petri dish/filter keeper, and wait for the scale to come back to zero before weighing the next filter.
- Repeat steps 2.4 and 2.5 and enter it as "Weight 2" in the CRF.
3. Microenvironment/personal air sampling
NOTE: A detailed outline of the instrumentation and steps involved in microenvironment/personal air sampling is given in Supplementary Figure 2.
- For personal monitoring, place the instruments in a vest (Figure 1 Ai) and advise the participant to wear it for 24 h, except during bathing and sleeping.
- During bathing and sleeping, instruct the participants to place the vest <1 m away on a customized metal stand (Figure 1Aii) provided by the field team.
- For microenvironmental monitoring, choose an appropriate location and place the metal stands with the instruments (Figures 1C,D; Supplementary Table 1) at 1.5 m above ground level, 1 m away from doors and windows if possible, and 1 m away from the combustion zone of the primary cookstove (when placed in kitchens).
- Perform a 5 min walkthrough in the monitoring area, record the START and END time for all the monitoring instruments (PM2.5, BC, CO, and time and location monitor) in the respective CRFs.
- On the removal day (Day 2, after 24 h), collect and wrap the instruments in aluminum foil and place it in a resealable cover for transport to the field office. Until removal of filter, place the ECM sampler in the cooler box (to maintain cold chain).
- PM2.5 measurement
NOTE: Use ECM, which is well suited for this application due to its small size (height: 12 cm; width: 6.7 cm) and weight (~150 g). The ECM collects nephelometric and gravimetric samples at 0.3 L/min (for up to 48 h) by drawing air through an impactor attached to a cassette containing 15 mm polytetrafluoroethylene filters19,26,27.- Clean all the ECM parts (inlet head, impactor pieces, U-shaped cassette lock) using an alcohol swab (70% isopropyl alcohol) and launch the sampler using ECM software (e.g., MicroPEM docking station).
- Place the calibration cap over the ECM's inlet and connect a flow meter with a HEPA filter to the calibration cap.
- After setting up the calibration assembly, press the Start button and wait 5 min for it to stabilize. Adjust the flow rate (within 5% of 0.3 L/min) and record in CRF-H48.
- Connect the HEPA filter directly to the ECM inlet, adjust the nephelometer offset until the value reads 0.0 and record the reading in CRF-H48.
- Set the program for 24 h and press the Submit Calibration Values button; the ECM is now ready for sampling.
- After sampling, leave the sampled ECMs at room temperature for a minimum of 20 min and record the post-sampling flow rate in CRF-H48. Download and save the ECM data using the filename convention.
- Remove the filter, place it in a filter keeper, and then store it at -20 °C.
- Black carbon (BC) measurement
- Use a transmissometer to measure the light attenuation through the filter at an 880 nm wavelength19,26,27.
- Switch on and stabilize for 15 min. Ensure that the correct-sized cartridges (i.e., 15 and 47 mm cartridges) are available in both the blank and sample slots of the BC instrument.
- Perform the scan on a neutral density (ND) and a blank filter with the assigned ID (Supplementary Figure 3 and Supplementary Table 2).
- After scanning the blank filter, place the lab blank into the sample cartridge slot above the sample diffuser and insert into the slot of the instrument at position 2.
- Remove the lab blank and continue the scan with test filters and sample filters.
- After completing the filter scan, remove the filter and return it to the Petri dish/filter keepers. Select the scanned data, click the Accept button, and then Save the data.
- Carbon monoxide (CO) measurement
NOTE: The CO instrument is small (about the size of a large pen), can log continuously for ~32,000 points, has a range of 0-1,000 ppm, and has been used to assess exposures and HAP in various other monitoring efforts19,26,27.- Start and set up the CO data logger for 1 min using the software. The screen shows 'CO logger has been configured successfully'. The instrument is ready for sampling.
- After sampling, open the CO logger using the software, press Stop to stop the USB data logger, and save the data after downloading.
- Calibrate the CO logger
- Set up the CO logger at the 1 min sampling rate and place it in the calibration box, with the inlet vent of the sensors facing toward calibration box's air inlet port.
- For 5 min, set a flow rate of 2 L/min of zero-grade air or room air. Make a note of the start and end time. Reduce the airflow to 1 L/min. Again make a note of the start and end time.
- Repeat the procedure with span gas (50-150 ppm standard of CO in zero-grade air), followed by zero-grade air as described in the previous step.
- Download the calibrated data to a specific folder. Open the calibration data file and enter the CO logger monitor's data into CRF-H47.
- Time and location logger (TLL)
NOTE: Use two types of Bluetooth instrument to monitor the time and location of the child. Have the child wear a vest containing two coin-sized time and location monitors (TLM), linked to a logger located near the ECMs and the mother's sampling vest, as shown in Figure 1Aiii. Calculate the child's exposures by integrating corresponding area concentrations over the time spent in that location19,26,27.- Charge the power bank and ensure that the logger is working by connecting with it.
- Time and location monitor (TLM)
- Insert a CR2032 battery into the monitor (lights should blink a few times if the battery has sufficient power).
- For the 'O' model TLM, press the soft cover to hear a click, and a green light should flash, indicating that the TLM is now 'ON' and transmitting its signal. For the 'EM' model TLM, press the soft cover to turn on the first mode (the light should flash green). Press again to get into the middle mode (light should flash green again).
- After sampling, download the data from the 'boot' drive that appears in the logger's SD card. Copy and save the files from the specified 'TLL' folder.
4. Stove use monitoring
- Collect details about stove usage patterns through surveys and the deployment of objective sensor-based measures. Place temperature loggers on both LPG and biomass stoves18,19,28. A detailed outline of the instrumentation and steps involved in stove use monitoring of data collection in the central lab, field lab, and field site activities are given in Supplementary Figure 4.
- Place the thermocouple probe near to the cumbersome zone of the cookstove, as shown in Supplementary Figure 5, and install the Dots.
- Open the Geocene app and enter the mission name, sampling interval, household ID, stove types, randomization details, campaign, tags, and notes. Press Start New Mission. Record the installation details in CRF-H40.
- Every 2 weeks, download the data using the app, and transfer over Bluetooth from the Dot to the cloud server. Record the information in CRF-H40.
5. Ambient monitoring
NOTE: The ambient PM2.5 instrument records real-time airborne PM2.5 and has an inbuilt 47 mm filter that can collect PM2.5 for gravimetric evaluation19,26,29. A detailed outline of the instrumentation and steps involved in ambient monitoring of data collection in the central lab, field lab, and field site activities are given in Supplementary Figure 6.
- Follow US EPA guidelines30 on the instrument and inlet placement: a) >2 m from walls; b) >10 m from trees; c) 2-7 m above the ground; and d) >2 m from roadways.
- Mount the ambient PM2.5 instrument on a concrete platform with earthing. Ensure there is no ambient background air pollution and enter the sampling details in CRF-H46.
- From the menu option, set the sampling interval to 5 min. Note the start time and perform flow calibration using a null filter. Collect real-time data for 6 days.
- On the start day of gravimetric sampling, download and save the real-time data.
- Remove the previously installed null filter and clean the filter holder using laboratory tissues. Place a pre-weighed filter and fill CRF-H46.
- After 24 h, stop the sampler and download the real-time data. Record the sampling information in CRF-H46. Remove the filter, wrap with aluminum foil, and place it into a resealable bag during cold chain transport.
6. Biomonitoring
- Urine sample collection, processing, and storage
NOTE: Follow the steps involved in collecting morning void urine samples in the participant's home according to US CDC guidelines19,31,32. Collect the urine samples from pregnant mothers (BL, P1, and P2 visits) and other adult women (BL, P1, P2, B1, B2, and B4 visits); in children (B1, B2, and B4 visits) with the administration of respective CRF-B10 on day 2. A detailed outline of the steps involved in biomonitoring in the central lab, field lab, and field site activities are provided in Supplementary Figure 7.- For the urine sample collection, provide the urine collection cup (M and OAW) on day 1. Similarly, instruct the mother to collect the child urine sample in the morning on the next day in a urine bag or directly into the cup and store it in a vaccine bag.
- At the field laboratory, store the collected urine samples between 1-8 °C. Before aliquoting, thaw the urine cup.
- To aliquot, process one urine sample at a time. Aspirate 2 mL of the sample and add into two 4 mL cryovials, 5 mL into two 10 mL cryovials, 15 mL into an archival tube, and store at -20 °C.
- The same procedure of aliquoting is followed for the field blank sample (water).
- DBS collection, drying, and storage
NOTE: Train the surveyors to collect DBSs via finger prick in pregnant mothers (BL, P1, and P2 visits) and other adult women (BL, P1, P2, B1, B2, and B4 visits), and heel prick or finger prick in children (B0, B1, B2, and B4 visits), following WHO recommendations33,34. A detailed procedure of DBS collection from M and OAW is provided in Annexure-H of the supplementary file.- For the child, collect the heel prick DBSs based on WHO guidelines, using the appropriate lancets.
- Choose the left or right heel, and wipe the puncture site with an alcohol swab.
- Keep the lancet in a horizontal position at the skin puncture location and prick. After pricking, wipe away the first drop of blood with a sterile cotton gauze.
- Place the capillary tube near the puncture site on the layer of the blood, and allow the blood to flow into the tube through capillary action.
- After filling enough blood volume in the capillary tube, immediately apply the blood within the circle of the protein saver card.
- Allow the specimen to air dry (overnight) in a horizontal direction at room temperature.
- Make sure the blood spots are a dark brownish color and no red areas are visible.
- After drying, place the DBS card in resealable bio-specimen bag containing desiccant (at least two sachets) with a humidity indicator card and store it at -20 °C.
7. Chain-of-custody (COC) of sampled filters
- Refer to the supplementary file for detailed steps. Steps explaining filter conditioning are described in Annexure A, microenvironment/personal air sampling of PM2.5 are present in Annexure B, BC measurement are described in Annexure C, CO measurement in Annexure D, time and location monitoring in Annexure E, stove use monitoring in Annexure F, ambient monitoring in Annexure G, biomonitoring in Annexure H, and sample transport in Annexure I. The list of CRFs used is given in Supplementary Table 3.
NOTE: Figure 2A shows the ECM collected after sampling and wrapped in aluminum foil. The wrapped filters were packed in separate biospecimen bags and placed in vaccine bags containing a pre-frozen gel pack. Sampled filters were transported to the field laboratory (Figure 2B). As shown in Figure 2C, filters transported from the field site were stored in a deep freezer (-20 °C) at the field laboratory and kept undisturbed until transported to the central laboratory. Every 15 to 30 days, samples were shipped by road to the central laboratory; sampled filters were packed on dry ice and gel packs with COC. Upon receiving the samples from the field office, the samples were cross-checked with the COC and archived in a deep freezer (-20 °C).
Representative Results
Microenvironment/personal air sampling methodologies:
Figure 1Ai shows a pregnant mother wearing the customized vest during the 24 h sampling period. The vest includes the ECM, CO logger, and time and location logger with the power bank. It was ensured that the participants wore the vest throughout the sampling period, except while bathing and sleeping. The stand that was provided to hang the vest within the sleeping periphery is shown in Figure 1Aii.
Figure 1Bi shows cleaning of the ECM sampler during the pre- and post-sampling period and Figure 1Bii shows the calibration of ECM in the field laboratory. The flow rates were checked and the sampling runtime was set prior to sampling, and any deviations were checked in the post-sampling period.
Figure 1C shows the instrument placement (ECM, CO logger, and TLL) in the kitchen (1.5 m height from the ground) for area monitoring. The instruments were placed and installed 1 m away from the cooking source. When windows or doors were near the sources, the instruments were installed 1 m away from these openings. Figure 1D shows the instruments (ECM, CO logger, and TLL) connected with a power bank, installed (1.5 m height from the ground) outdoors in each participants' house. The results of microenvironmental and personal PM2.5 following these methodologies are already published24,35,36.
The data of CO logger calibration over 1 year showed low malfunctions, as shown in Supplementary Figure 8 (legend shown as a circle represents the measurement of the CO data logger reads beyond the calibration range of 0-50 ppm)35. Details about the difference between the blank and sample slot of BC measurement for loading the filter is given in the supplementary material (Annexure C).
Figure 1Ei illustrates damaged filters before the pre-weighing process. Damaged and dropped filters are flagged as invalid. Filters were rechecked at the field laboratory before loading into any air monitoring instruments. Similarly, sampled filters were examined for any damage, such as holes, tears, stretching, or dislodgment, as given in Figure 1Eii. If any such damage existed, it was weighed, but not considered as valid for subsequent analyses. PM2.5 mass for each sample was obtained by subtracting the sample mass from the median field blank mass. The final PM2.5 concentration was estimated by dividing the blank corrected filter masses by the amount of air sampled by the pump during the measurement interval. The derived threshold criteria for valid PM2.5 and CO sampling is given in Table 1. Data within the threshold criteria are considered valid and taken up for the analysis.
Stove use monitoring
Figure 3A shows the calibration of temperature loggers, which was done initially on ice and then in hot water with the help of a standard temperature monitor. Figure 3Bi shows the regular pattern of peaks which are considered valid and identified by characteristic peak color (orange) when the stove is used. As shown in Figure 3B, the irregular pattern of peaks, such as (ii) probe problem (recording high temperatures and measuring beyond the temperature range), (iii) technical error (baseline shift with negative values), and (iv) thermocouple problem, was characterized as invalid sampling (no records of temperature measurement; baseline shift together with negative values). The temperature logger installed in different cookstoves is illustrated in Supplementary Figure 5. The results of stove use monitoring following this methodology is already published18,19,36.
Ambient air sampling
With US EPA guidelines (https://www.epa.gov/environmental-topics/air-topics), the ambient samplers were installed at the top of one of the selected households in each representative HAPIN-India site (Figure 4A). Sampling sites were chosen based on security, availability of electricity, and willingness of the participant to host the monitor. Sites were selected to be in central areas relative to clusters of participants. Ambient samples followed a similar procedure of packing and shipping from the field site to the field laboratory to the central laboratory. To prevent cables from being plugged into the incorrect connector, connect with the unique pin layout as given in Supplementary figure 9. The results of ambient monitoring (PM2.5) measured between 2018 to 2020 is shown in Figure 4B. Also, the results of ambient monitoring using this method elsewhere is already published29.
Biomonitoring
Figure 5A displays the urine aliquoting procedure. The samples from the field site were stored in vaccine cooler bags and transported to the field laboratory, where they were aliquoted and stored in a deep freezer (-20 °C). Figure 5B summarizes the sample collection, transport, and field storage COC.
Figure 5C shows the DBSs; 5Ci shows valid spots before drying, and 5Cii shows valid spots after drying. Table 2 summarizes the pattern of valid DBS collection in follow-up visits among the HAPIN participants (M, OAW, C). The success rate of collecting valid DBSs from mothers for three visits is 100% (BL), 93% (P1), and 83% (P2). Similarly, for OAW, the success of DBS collection was consistent (100%-72%) for the first three (BL-P2) visits, but reduced (45%-35%) from B1 to B4 during the pandemic and during hurricane Gaja (2018). The success of DBS collection in children was 72.09% at birth (B0), 64% at B1, 62% at B2, and 45% at B4.
Figure 5D emphasizes that the cold chain with dry ice maintains sample integrity. Every month, biological samples were packed with dry ice in a separate thermal insulation box and shipped with temperature and relative humidity (RH) loggers. Correlation analysis of urinary specific gravity measured between the field laboratory and central laboratory showed good agreement, as shown in Figure 5E. Our results of biomonitoring method cross-validation in urine samples of polycyclic aromatic hydrocarbon metabolites shows the quality assurance (QA)/quality control (QC) of sample integrity21.
All sampling and CRF data were securely uploaded from SRIHER to Emory University's server. Data transfer occurred daily, thus reducing the likelihood of data loss. The list of CRFs used for data collection are given in Supplementary Table 3. The data collection flow from the field site to the Emory server is given in Supplementary Figure 10.

Figure 1: Personal and microenvironmental monitoring. (A) i) Pregnant mother wearing the vest with air sampling instruments (ECM, CO logger, and TLL); ii) Metallic stand with the vest; iii) Child vest with TLM units. (B) i) ECM cleaning; ii) ECM calibration. (C) Kitchen area monitoring with the ECM, CO logger, and TLL. (D) Outdoor area monitoring with the ECM, CO logger and TLL. (E) i) Damaged pre-weighed filters; ii) Damaged sampled filters. Please click here to view a larger version of this figure.
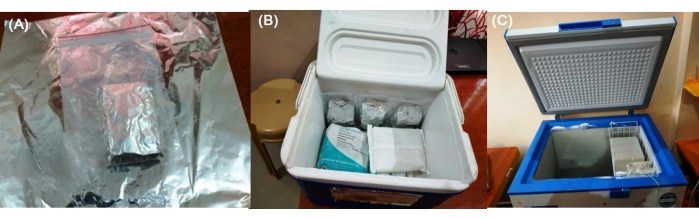
Figure 2: Chain-of-custody of filters. (A) Sampled ECM with filters wrapped up in aluminium foil. (B) Transport of sampled filters from participant households to the field lab in vaccine cooler bags containing gel packs. (C) Sample filters stored in a deep freezer (-20 °C) in the field laboratory. Please click here to view a larger version of this figure.
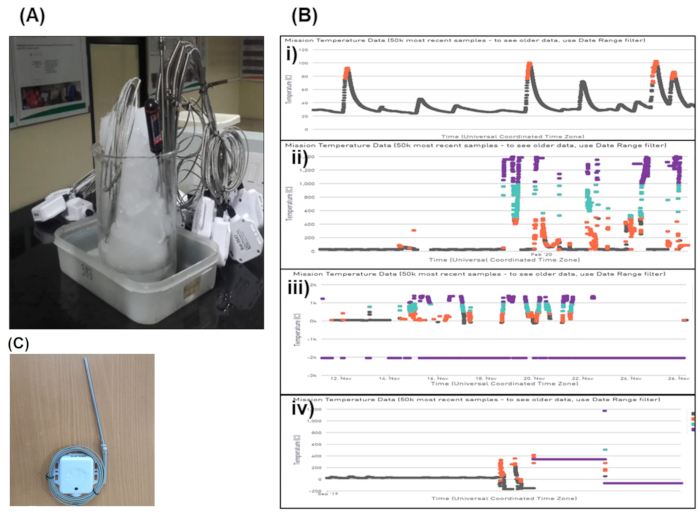
Figure 3: Stove use monitoring-temperature Loggers. (A) Calibration of Geocene Dot temperature loggers. (B) i) Valid pattern of peak for stove use monitoring; ii) Probe problem; iii) Technical error; iv) Thermocouple problem. (C) Stove use monitoring-Temperature Loggers. Please click here to view a larger version of this figure.

Figure 4: Ambient monitoring. (A) Ambient PM2.5 instrument installed at the field site. (B) Time series of ambient PM2.5 level measurements (2018-2020). Please click here to view a larger version of this figure.
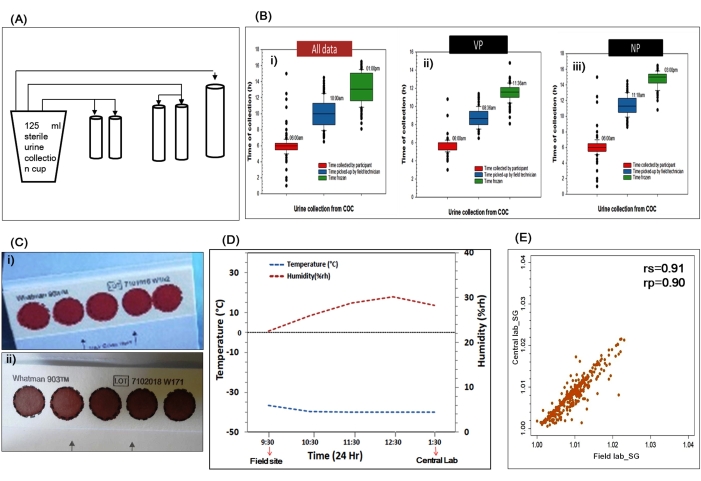
Figure 5. Biomonitoring-sample collection, processing, and quality control. (A) Urine aliquoting. (B) Chain-of-custody for sample collection, storage, and transport. (C) Dried blood spot: i) before drying; ii) after drying. (D) Cold chain-of-custody of sample shipment. (E) QA/QC of sample integrity-data of urinary specific gravity measured in the field site and central laboratory. Please click here to view a larger version of this figure.
Table 1: Valid sampling threshold criteria of PM2.5 and CO monitors. Note that due to sensitivity of the accelerometer, values outside of expected ranges were flagged but not excluded from analyses. Please click here to download this Table.
Table 2: Summary of valid DBS collection among the study participants. *During a hurricane (cyclone) there was a drop in DBS collection. †During COVID19 lockdown there was a drop in DBS collection. ‡During COVID19 lockdown there was a drop and 2021 data is not included in DBS collection. Abbreviations: M = pregnant mother; OAW = other adult woman; C = child. Please click here to download this Table.
Supplementary Table 1: Guidelines for the installation of samplers for microenvironmental monitoring.
Supplementary Table 2: Difference between the blank slot and sample slot for loading the filter. *The diffuser can be replaced only if there is any visible damage or if used for ~750-1,000 filters.
Supplementary Table 3: List of CRFs in respect to exposure and biomarker sampling. The CRFs are available in the RedCap database, stored at Emory University, and are maintained with the data-sharing agreement between all the collaborators, which can be provided to the readers upon request.
Supplementary Figure 1: Data entry sheet for filter weighing. Please click here to download this File.
Supplementary Figure 2. Instruments and steps involved in microenvironment and personal air sampling. Please click here to download this File.
Supplementary Figure 3: Cartridges and filter slots. A: Blank slot (Position 1); B: Blank bottom cartridge containing both the blank diffuser and the blank filter in the cartridge; C: Top piece of the blank cartridge; D: Sample slot (Position 2); E: Bottom sample cartridge with sample diffuser; F: Top piece of the sample cartridge. Please click here to download this File.
Supplementary Figure 4: Instruments and steps involved in stove use monitoring. Please click here to download this File.
Supplementary Figure 5: Dots installed in different cookstoves. Please click here to download this File.
Supplementary Figure 6: Instruments and steps involved in ambient air monitoring. Please click here to download this File.
Supplementary Figure 7: Instruments and steps involved in biological sampling. Please click here to download this File.
Supplementary Figure 8: Summary-of-summary of carbon monoxide (CO) data logger. Please click here to download this File.
Supplementary Figure 9: E-sampler connector layout. Please click here to download this File.
Supplementary Figure 10: Data collection and processing. Please click here to download this File.
Supplementary Figure 11: Usage of vaccine bag. Please click here to download this File.
Supplementary Figure 12: Difference between pelican and vaccine bag. Temperature performance of two cooler bags (pelican vs. vaccine) are tested using a CO data logger monitor for 48 h in the laboratory at an average room temperature of 28.3 ± 0.6 °C and RH of 49.2% ± 3.6%. A urine sample (~60 mL) with an initial temperature of 36.4 °C was placed in two bags and kept undisturbed for 48 h in a storage room. Please click here to download this File.
Discussion
We demonstrated and visually represented standard procedures to collect population-level data on personal exposures to household air pollution in the multi-country HAPIN trial19, 24. The field-based environmental and biomarker sampling methods described here are appropriate and feasible, particularly in vulnerable populations in resource-limited settings where PM2.5 exposures are several orders of magnitude higher than the WHO Air Quality Guideline (AQG) values (annual mean of 5 µg/m3 and 24 h mean of 15 µg/m3)37,38.
The instruments used in this study have been deployed in other studies with different sampling durations. In Jack et al., CO was measured every 6 weeks using a lightweight CO logger monitor, and PM2.5 measurement (microPEM) was co-located for 72 h on nearly half of pregnant participants9. Another study used ambient-adjusted personal exposures assessed with the Ultrasonic Personal Aerosol Sampler (UPAS) to address uncertainty in estimates of global impacts of HAP on cardiac health using a quantitative assessment of PM2.5 exposure14.
The procedures followed during the HAPIN trial and described here can serve as guidelines for personal/microenvironment HAP monitoring in other settings24,26. The field team first evaluated possible locations for placing the monitors in the kitchen, when sleeping, and in outdoor household locations. When there were no ideal conditions for placing the monitors (1.5 m above ground, 1 m away from the stove and any doors and windows), suitable places adjacent to the ideal sample location were chosen35. This occurred relatively infrequently-in <2% of all collected samples. Temperature loggers used as stove use monitors had waterproof covers to protect from spillage during kitchen activities, like cooking and heating water. However, temperature loggers that were placed on outdoor stoves were damaged during the monsoon and flooding (Figure 3C).
The compliance of wearing the vest was observed by field surveyors on the day of removing the monitors (Day 2). Compliance assessed via sensors was shown to be, at times, incorrect; in some instances, participants would be wearing the monitor, but would be sitting still and thus would be flagged as non-compliant. This recognition of sensor-based misclassification was only possible due to observant fieldworkers. As an additional check, our CRFs contained participant-reported compliance.
The handling of filters during conditioning, weighing, sampling (pre- and post-), transportation, and storage at the field and central laboratory are critical activities within any data collection phase. After 24 h of sampling, the personal monitor was completely covered in aluminium foil and placed in a biospecimen bag to transport in a cold chain and dust free environment. The current study has demonstrated the procedures for preserving the filters from the participants' home to the field laboratory to the central laboratory via chain-of-custody.
Few deviations from required temperature conditions during storage and transport are predicted during biological sample collection and transport from the field to the laboratory for analysis, which might lead to erroneous results. The cooler bag used in the multi-country installations were too expensive in India. Under various national programs in India, the vaccine cooler bag has been used widely used for vaccine transport. These vaccine bags were obtained locally at a reasonable cost, almost 30-fold lower than the cooler bag (Supplementary Figure 11). Before making a bulk purchase, the shipment temperature in these vaccine cooler boxes was compared with the cooler bag to ensure sample integrity (Supplementary Figure 12). In resource-constrained settings, collecting biological samples and maintaining their integrity is difficult. Transporting the samples in locally available vaccine bags from the participant's home to the field laboratory resolved this issue.
DBS collection is also known as spots of capillary blood obtained from a finger, heel, or ear lobe39. Using a DBS card for collecting blood samples is relatively painless and non-invasive, and can be collected in the participant's home through non-clinical but trained health personnel. The blood collected on the filter paper is easily dried and stored. A drop of whole blood occupies approximately 50 µL in a disc with a 12.7 mm diameter23. The ring finger is usually the preferred site for adults, and it is a common procedure in therapeutic monitoring. Although the steps involved in DBS collection for adult biomarker screening were visualized in earlier studies, the tasks and microsteps involved in resource-constrained settings have not been captured40,41. This study is among the first, to our knowledge, to capture DBSs from M, OAW, and C,) of the same household42. In rural settings, it is challenging, although the procedure is minimally invasive42. Frequent training for field surveyors about collecting valid DBSs, and technical clarifications on selecting the non-dominant hand, relaxing and massaging the arm, and selecting the ring or middle finger played a significant role in collecting valid DBSs33.
Similarly, for neonates, the capillary sampling through heel prick was performed for babies weighing from ~3 to 10 kg (birth to 6 months), and finger prick in follow-up (over 6 months) for babies weighing >10 kg. Following WHO guidelines, the choice and position (puncture at a 90° angle parallel to the heel) of the lancet for pricking has played a significant role in obtaining enough blood flow, successful collection of DBSs, and a slightly shorter estimated depth33,34. The length of the blade in a lancet varies by manufacturer (i.e., from 0.85-2 mm for neonates). In premature babies, lancets for heel prick (0.85 mm x 1.75 mm depth) and lancets for finger-prick (1 mm x 2.5 mm depth) were utilized with babies between 6 months and 8 years.
After heel prick, the blood wass drawn using PTS capillary tubes (Ref# 2866) to collect the sample without clots in the blood spots and to avoid stamping on the protein saver card. Based on our preliminary experiments, it is believed that placing the capillary tube downward takes up the blood promptly without any hindrances due to uniform surface tension.
Following the successful collection of valid DBSs from HAPIN participants in both the study sites, the sample collected in the protein saver card was dried overnight at room temperature (25 °C) in the field laboratory, and it was ensured that the protein saver card was free of any insects and houseflies by a covering insect net. After drying (brown color, Figure 5Cii), the DBS card was stored at -20 °C.
During the DBS collection at participants' homes, the dropped blood was within 12.7 mm spot, but after drying overnight at room temperature, the two individual spots became merged, in the NP site. The observed difference in the NP site might be due to the higher relative humidity, where the collected valid DBSs became invalid as the two individual dry blood spots became fused. Following the harmonized DBS collection procedure, the results of clinical biomarkers (oxidative stress, inflammation, endothelial dysfunction, lung insult) have been cross-validated on blinded samples in the LEADER laboratory at Emory University, and were found to be in good agreement (data not shown).
Biospecimen collection requires firm adherence to safety protocols. During the pandemic period (March 24, 2019 to June 2019), additional safety protocols were executed, following the advisories of the local government. The study staff was instructed to wear personal protective equipment (PPE) such as gloves, face masks, goggles, and aprons while traveling and in participant houses. Lab coats were mandatory while working in field offices, and field offices were equipped with biosafety cabinets for handling biospecimens. Training was provided to all staff on using and identifying damaged PPEs. The used PPEs were collected in separate disposal bags and handed over at the collaborating health centers for safe disposal to the common biomedical waste management facility authorized by the State Pollution Control Board.
Capturing high-resolution videos of field data collection, especially in challenging rural settings, will aid in bridging the training gaps in air pollution monitoring and field data collection. Overall, at every stage of project execution, the quality and reliability of data collection was ensured. Periodical trainings and retrainings of field staff built their capacity and confidence and avoided the expensive loss of sample integrity. The methods used are transferable and will assist other researchers in adopting environmental monitoring and biospecimen collection procedures in LMICs using cost-effective strategies.
The gaps and challenges faced throughout the HAPIN study, particularly in resource-limited rural areas, are also reported. We note that extensive preliminary work and training, reported elsewhere in publications detailing HAPIN's formative work, were critical for sorting out issues with the protocol, like the design of vests for sampling and the mechanisms for safe transport of both air pollution and biological specimens. Furthermore, during this period, many 'growing pains' were overcome, including handling of the very small 15 mm ECM gravimetric filters, techniques for placement of stove use monitors, etc.
Special attention was made while shipping the sampled filters, instruments, and biospecimens from households to the field laboratory. All air sampling equipment, accessories, and samples were tracked through inventory management at the central and field laboratories. It has allowed timely maintenance, repair, replacement, and evaluation of project supplies to provide uninterrupted data collection.
The data collection methods demonstrated here have proved reliable and consistent during the entire year-long study period. The use and adoption of affordable and smart technologies may point toward a future paradigm for randomized control trials (RCTs) and exposure-response studies, ensuring acceptable data collection to yield reliable results. Such endeavors are not without their challenges; however, as shown here, diligence and review of established protocols can ensure that field teams are able to adapt to changing circumstances, both expected (differences in household configurations, for example) and unexpected (COVID-19, hurricanes). For HAPIN, this began with hands-on training in the laboratory and the field provided by exposure and biomarker core experts prior to the trial. In addition, refresher training was given once every 6 months at various tiers throughout the study period. The periodic coaching increased the team's ability to efficiently sample and handle instruments, filters, and biospecimens. The visualization and field sampling procedures will be a valuable educational tool for researchers conducting similar large-scale epidemiological studies in India or LMICs.
Offenlegungen
The authors have nothing to disclose.
Acknowledgements
The investigators would like to thank the members of the advisory committee – Patrick Brysse, Donna Spiegelman, and Joel Kaufman – for their valuable insight and guidance throughout the implementation of the trial. We also wish to acknowledge all research staff and study participants for their dedication to and participation in this important trial.
This study was funded by the U.S. National Institutes of Health (cooperative agreement 1UM1HL134590) in collaboration with the Bill & Melinda Gates Foundation (OPP1131279). A multidisciplinary, independent Data and Safety Monitoring Board (DSMB) appointed by the National Heart, Lung, and Blood Institute (NHLBI) monitors the quality of the data and protects the safety of patients enrolled in the HAPIN trial. NHLBI DSMB: Nancy R. Cook, Stephen Hecht, Catherine Karr (Chair), Joseph Millum, Nalini Sathiakumar, Paul K. Whelton, Gail Weinmann and Thomas Croxton (Executive Secretaries). Program Coordination: Gail Rodgers, Bill & Melinda Gates Foundation; Claudia L. Thompson, National Institute of Environmental Health Science; Mark J. Parascandola, National Cancer Institute; Marion Koso-Thomas, Eunice Kennedy Shriver National Institute of Child Health and Human Development; Joshua P. Rosenthal, Fogarty International Center; Conception R. Nierras, NIH Office of Strategic Coordination Common Fund; Katherine Kavounis, Dong- Yun Kim, Antonello Punturieri, and Barry S. Schmetter, NHLBI.
HAPIN Investigators: Vanessa Burrowes, Alejandra Bussalleu, Devan Campbell, Eduardo Canuz, Adly Castañaza, Howard Chang, Yunyun Chen, Marilú Chiang, Rachel Craik, Mary Crocker, Victor Davila-Roman, Lisa de las Fuentes, Oscar De León, Ephrem Dusabimana, Lisa Elon, Juan Gabriel Espinoza, Irma Sayury Pineda Fuentes, Dina Goodman, Meghan Hardison, Stella Hartinger, Phabiola M Herrera, Shakir Hossen, Penelope Howards, Lindsay Jaacks, Shirin Jabbarzadeh, Abigail Jones, Katherine Kearns, Jacob Kremer, Margaret A Laws, Pattie Lenzen, Jiawen Liao, Fiona Majorin, McCollum, John McCracken, Julia N McPeek, Rachel Meyers, Erick Mollinedo, Lawrence Moulton, Luke Naeher, Abidan Nambajimana, Florien Ndagijimana, Azhar Nizam, Jean de Dieu Ntivuguruzwa, Aris Papageorghiou, Usha Ramakrishnan, Davis Reardon, Barry Ryan, Sudhakar Saidam, Priya Kumar, Meenakshi Sundaram, Om Prashanth, Jeremy A Sarnat, Suzanne Simkovich, Sheela S Sinharoy, Damien Swearing, Ashley Toenjes, Jean Damascene Uwizeyimana, Viviane Valdes, Kayla Valentine, Amit Verma, Lance Waller, Megan Warnock, Wenlu Ye.
Materials
| BD adult lancet | BD Biosciences | 366594 | DBS collection from finger |
| BD Quikheek infant safety lancet | BD Biosciences | 368100 & 368101 | Heel prick DBS collection |
| Beacon | Roximity | O/EM | Time and location monitor [TLM] (Personal monitor) |
| Beacon Logger | Berkley Air Monitoring group | xxxx | Time and location logger [TLL] (Indirect measurement) |
Cr do ProMed Pelican Bag do ProMed Pelican Bag |
Peli Biothermal USA | Cooler bag | |
| Enhanced Children MicroPEM (ECM) | RTI International, Durham, NC, US | xxxx | Personal monitor of PM2.5 |
| E-sampler | Met One Instruments | 9800 | Indirect measurement of ambient PM2.5 |
| Geocene | Geocene Inc., Vallejo,CA | xxxx | for stove use monitoring |
| Humidity indicating card | DESSICARE, INC. | 04BV14C10 | Sample integrity indicator |
| Lascar | Lascar Electronics | EL-USB-300 | Carbon monoxide (CO) data logger |
| PTS collect capillary tubes- 40 µL | PTS collect | 2866 | To collect heel prick DBS from children |
| Sartorius | Sartorius Lab Instruments, GmbH & Co, Germany | MSA6-6S-000-DF | Microbalance (Weighing filters) |
| SootScanTM | Magee Scientific Co, Berkeley, USA | OT21 | Black carbon measurement |
| Vaccine Bag | Apex International, India | AIVC-46 | Vaccine Bag |
| Whatman 903 Protein Saver card | GE Healthcare Life Sciences | 10534612 | Collection of capillary blood samples (Dried Blood Spot) |
Referenzen
- Odo, D. B., Yang, I. A., Knibbs, L. D. A systematic review and appraisal of epidemiological studies on household fuel use and its health effects using demographic and health surveys. International Journal of Environmental Research and Public Health. 18 (4), 1411 (2021).
- Pope, D., et al. Are cleaner cooking solutions clean enough? A systematic review and meta-analysis of particulate and carbon monoxide concentrations and exposures. Environmental Research Letters. 16 (8), 083002 (2021).
- Smith, K. R., Pillarisetti, A. Household air pollution from solid cookfuels and its effects on health. Injury Prevention and Environmental Health. , (2017).
- Balakrishnan, K., et al. Air pollution from household solid fuel combustion in India: an overview of exposure and health related information to inform health research priorities. Global Health Action. 4 (1), 5638 (2011).
- Balakrishnan, K., et al. State and national household concentrations of PM2.5 from solid cookfuel use: Results from measurements and modeling in India for estimation of the global burden of disease. Environmental Health. 12 (1), 77 (2013).
- Corsi, D. J., et al. Prospective Urban Rural Epidemiology (PURE) study: Baseline characteristics of the household sample and comparative analyses with national data in 17 countries. American Heart Journal. 166 (4), 636-646 (2013).
- Keller, J. P., et al. A hierarchical model for estimating the exposure-response curve by combining multiple studies of acute lower respiratory infections in children and household fine particulate matter air pollution. Environmental Epidemiology. 4 (6), 119 (2020).
- Arku, R. E., et al. Characterizing exposure to household air pollution within the Prospective Urban Rural Epidemiology (PURE) Study. Environment international. 114, 307-317 (2018).
- Jack, D. W., et al. Ghana randomized air pollution and health study (GRAPHS): study protocol for a randomized controlled trial. Trials. 16 (1), 420 (2015).
- Liang, L., et al. Assessment of personal exposure to particulate air pollution: The first result of City Health Outlook (CHO) project. BMC Public Health. 19 (1), 711 (2019).
- Chowdhury, S., et al. Indian annual ambient air quality standard is achievable by completely mitigating emissions from household sources. Proceedings of the National Academy of Sciences. 116 (22), 10711-10716 (2019).
- Checkley, W., et al. Effects of a household air pollution intervention with liquefied petroleum gas on cardiopulmonary outcomes in Peru. A randomized controlled trial. American Journal of Respiratory and Critical Care Medicine. 203 (11), 1386-1397 (2021).
- Ranzani, O. T., et al. Association between ambient and household air pollution with carotid intima-media thickness in peri-urban South India: CHAI-Project. International Journal of Epidemiology. 49 (1), 69-79 (2020).
- Ranzani, O. T., et al. Personal exposure to particulate air pollution and vascular damage in peri-urban South India. Environment International. 139, 105734 (2020).
- Balakrishnan, K., et al. Establishing integrated rural-urban cohorts to assess air pollution-related health effects in pregnant women, children and adults in Southern India: an overview of objectives, design and methods in the Tamil Nadu Air Pollution and Health Effects (TAPHE) study. BMJ Open. 5 (6), 008090 (2015).
- Shupler, M., et al. Multinational prediction of household and personal exposure to fine particulate matter (PM2.5) in the PURE cohort study. Environment International. 159, 107021 (2022).
- Smith, K. R. Effect of reduction in household air pollution on childhood pneumonia in Guatemala (RESPIRE): A randomised controlled trial. The Lancet. 378 (9804), 1717-1726 (2011).
- Pillarisetti, A., et al. Patterns of stove usage after introduction of an advanced cookstove: The long-term application of household sensors. Environmental Science and Technology. 48 (24), 14525-14533 (2014).
- Johnson, M. A., et al. Air pollutant exposure and stove use assessment methods for the household air pollution intervention network (HAPIN) trial. Environmental Health Perspectives. 128 (4), 047009 (2020).
- Barr, D. B., Wang, R. Y., Needham, L. L. Biologic monitoring of exposure to environmental chemicals throughout the life stages: requirements and issues for consideration for the National Children’s Study. Environmental Health Perspectives. 113 (8), 1083-1091 (2005).
- Puttaswamy, N., et al. Cross-validation of biomonitoring methods for polycyclic aromatic hydrocarbon metabolites in human urine: Results from the formative phase of the household air pollution intervention network (HAPIN) trial in India. Journal of Chromatography B. 1154, 122284 (2020).
- Barr, D. B., et al. Urinary creatinine concentrations in the U.S. population: implications for urinary biologic monitoring measurements. Environmental Health Perspectives. 113 (2), 192-200 (2005).
- McDade, T. W., Williams, S., Snodgrass, J. J. What a drop can do: dried blood spots as a minimally invasive method for integrating biomarkers into population-based research. Demography. 44 (4), 899-925 (2007).
- Sambandam, S., et al. Exposure contrasts associated with a liquefied petroleum gas (LPG) intervention at potential field sites for the multi-country household air pollution intervention network (HAPIN) trial in India: Results from pilot phase activities in rural Tamil Nadu. BMC Public Health. 20 (1), 1799 (2020).
- Clark, S. N., et al. High-resolution spatiotemporal measurement of air and environmental noise pollution in Sub-Saharan African cities: Pathways to equitable health cities study protocol for Accra, Ghana. BMJ Open. 10 (8), 035798 (2020).
- Clasen, T., et al. Design and rationale of the HAPIN study: A multicountry randomized controlled trial to assess the effect of liquefied petroleum gas stove and continuous fuel distribution. Environmental Health Perspectives. 128 (4), 47008 (2020).
- Liao, J., et al. LPG stove and fuel intervention among pregnant women reduce fine particle air pollution exposures in three countries: Pilot results from the HAPIN trial. Environmental Pollution (Barking). 291, 118198 (2021).
- Wilson, D. L., Williams, K. N., Pillarisetti, A. An integrated sensor data logging, survey, and analytics platform for field research and its application in HAPIN, a multi-center household energy intervention trial. Sustainability. 12 (5), 1805 (2020).
- Rooney, B., et al. Impacts of household sources on air pollution at village and regional scales in India. Atmospheric Chemistry and Physics. 19 (11), 7719-7742 (2019).
- Review of the National Ambient Air Quality Standards for Particulate Matter. Environmental Protection Agency Available from: https://www.epa.gov (2020)
- Barr, D. B., et al. Design and rationale of the biomarker center of the household air pollution intervention network (HAPIN) trial. Environmental Health Perspectives. 128 (4), 47010 (2020).
- Cross Sectional Assessment Study Appendix D, biologic sample collection and analysis plans. CDC/NCEH Available from: https://www.cdc.gov/inceh/clusters/fallon/6_ApdxD_Biomethods.pdf (2022)
- Practical guidance on capillary sampling (finger and heel-prick). World Health Organization Available from: https://cdn.who.int/media/docs/default-source/integrated-health-sevices-(his) (2010)
- WHO guidelines on drawing blood: best practices in phlebotomy. World Health Organization Available from: https://apps.who.int/iris/handle/10665/44294 (2010)
- Johnson, M., et al. Exposure contrasts of pregnant women during the household air pollution intervention network randomized controlled trial. Environmental Health Perspectives. 130 (9), 097005 (2022).
- Piedrahita, R., et al. Exposures to carbon monoxide in a cookstove intervention in northern Ghana. Atmosphere. 10 (7), 402 (2019).
- Balakrishnan, K., Cohen, A., Smith, K. R. Addressing the burden of disease attributable to air pollution in india: the need to integrate across household and ambient air pollution exposures. Environmental Health Perspectives. 122 (1), 6-7 (2014).
- Air quality monitoring, emission inventory and source apportionment study for Indian cities. Central Pollution Control Board Available from: https://www.epa.gov (2011)
- Stove, C. P., Ingels, A. -. S. M. E., De Kesel, P. M. M., Lambert, W. E. Dried blood spots in toxicology: from the cradle to the grave. Critical Reviews in Toxicology. 42 (3), 230-243 (2012).
- Grüner, N., Stambouli, O., Ross, R. S. Dried blood spots – preparing and processing for use in immunoassays and in molecular techniques. Journal of Visualized Experiments. (97), e52619 (2015).
- Ostler, M. W., Porter, J. H., Buxton, O. M. Dried blood spot collection of health biomarkers to maximize participation in population studies. Journal of Visualized Experiments. (83), e50973 (2014).
- Shan, M., et al. A feasibility study of the association of exposure to biomass smoke with vascular function, inflammation, and cellular aging. Environmental Research. 135, 165-172 (2014).

