골반 시험 I: 외부 생식기의 평가
English
分享
概述
근원:
알렉산드라 던컨, GTA, 프액시스 임상, 뉴 헤이븐, CT
티파니 쿡, GTA, 프랙시스 임상, 뉴 헤이븐, CT
자이딥 S. 탈워더,MD, 내과 및 소아과, 예일 의과 대학, 뉴 헤이븐, CT
골반 검사는 환자에게 침습적이라고 느낄 수 있으므로 환자가 취약하기보다는 편안하고 힘을 느낄 수 있도록 가능한 모든 것을 하는 것이 중요합니다. 임상의는 구두와 비언어적으로 의사 소통방법을 알고 있어야하며 가능한 한 환자에게 통제할 수 있어야합니다. 시험 테이블이 어떻게 시험 내내 관여하는지에 이르기까지 여러 가지 방법이 있습니다. 5명의 환자에 대하여 1만큼 성적인 외상을 경험했을 지도 모릅니다; 따라서, 그 환자를 트리거하지 않는 것이 중요하지만, 그들이 누구인지 알 수있는 것은 항상 불가능하다. 이 비디오의 시험은 가능한 최상의 경험을 만들기 위해 모든 환자와 함께 사용할 수있는 중립적 인 언어와 기술을 보여줍니다.
가능한 한 환자를 덮고 외부 접촉을 최소화하는 것이 중요합니다. 임상의는 음핵 또는 항문과의 우발적 인 접촉을 피하기 위해 환자를 검사하는 데 사용되지 않는 손가락을 감싸야합니다.
골반 검사를 수행하기 전에, 심사관은 환자가 시험과 자신의 몸에 대해 얼마나 지식이 있는지 알아 내고 환자가 시험 내내 질문이나 우려를 전달할 수 있다는 기대를 확립해야합니다. 매우 임상적인 언어를 피하는 것이 항상 중요하지만, 특정 구어체 단어는 이 시험 중에 돌보는 것에서 지나치게 친밀한 단어로 선을 넘을 수 있습니다. 이러한 맥락에서 성적 느낌을 느낄 수 있는 “터치”와 “느낌”이라는 단어를 피하는 것이 도움이 됩니다. 대신 “평가”, “확인”, “검사” 또는 “검사”라는 단어를 사용해야 합니다. “침대”와 “시트”라는 단어는 피해야 하며 대신 “테이블”과 “커튼”을 사용해야 합니다. 또한 임상의는 말을 혼동하지 않도록 “스트럽”이 아닌 “발판”이라는 단어를 사용해야 합니다. 환자가 불안할 때 따르는 것이 어렵기 때문에 환자에게 “이완”을 말하는 것을 피하는 것이 좋습니다. 환자에게 특정 근육을 “부드럽게” 또는 “방출”하도록 요청하는 것이 더 유용할 수 있으며, 환자가 케겔 운동이나 Valsalva 기동을 하는 것이 특정 이완 기술로 작용할 수 있습니다.
모범 사례는 여성 해부학 환자가 다른 성별 (예 : 트랜스젠더 또는 성별 키커)으로 식별 할 수 있기 때문에 환자의 성별에 대한 가정을 피하는 것을 지시합니다. 이 비디오는 그의 역사가 부인과 건강과 관련된 특정 불만 이나 위험 요소를 밝히지 않은 환자에 대한 접근 방식을 묘사합니다.
골반 시험은 외부 생식기의 시각 및 수동 시험, 관중 시험 및 양수동 시험의 세 부분으로 구성됩니다. 이 비디오는 골반 시험과 외부 생식기 시험에 대한 소개를 다룹니다. 잠재적인 발견을 놓치지 않으려면 외음부(그림1)의육안 검사와 땀샘과 톤의 내부 심근 및 평가라는 두 가지 주요 구성 요소로 구성된 체계적인 접근 법으로 외부 골반 시험을 수행해야 합니다.
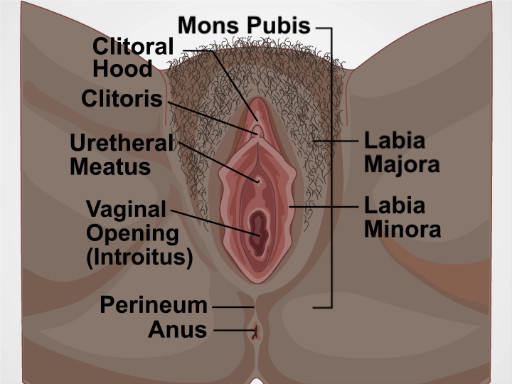
그림 1. 외음부의 다이어그램입니다. 외부 성기를 표시하는 다이어그램으로 표시되어 있습니다.
Procedure
Applications and Summary
This video reviewed the introduction and setup for the pelvic exam, and how to visually inspect and examine the complete female external genitalia. Before performing the pelvic exam, examiners should find out how knowledgeable the patients are about the exam and their own bodies, and establish the expectation that the patients can communicate questions or concerns throughout the exam. The exam table should be positioned so the patient can see what is happening and can communicate with the examiner, and the patient should remain covered as much as possible to minimize feelings of vulnerability. The examiner can give the patient a hand mirror and instruct how to position it to follow along with the exam, and educate the patient about their structures throughout the exam (when appropriate).
The examiner should first provide an overview of the exam, and explain every step as the exam progresses, letting the patient know before the examiner makes contact with the patient's genitalia. First, the external genitalia is examined, including the glands and muscle tone of the vagina. The examiner should take note of any potential findings (including taking swabs of any unusual discharge elicited). Any markings or potential signs of domestic or intimate partner violence should be documented, though examiners should remember that some of their patients may engage in rough sex, and bruising may not be indicative of violence.
Beyond asking clarifying questions, the examiner should not discuss concerns or follow-up testing while the exam is ongoing. Following the components covered in this video, the pelvic examination is typically followed by two additional components, the speculum and bimanual exams. After the speculum and bimanual exams, the examiner should step out to allow the patient to get dressed. The examiner can then reenter the room to discuss concerns and next steps, as having those conversations while the patient is unclothed and vulnerable heightens anxiety.
When an exam has normal findings, the examiner should always tell the patient that "everything appears healthy and normal." This simple statement relieves anxiety and empowers patients to equate their body structures as normal.
References
- Black M.C., Basile K.C., Breiding M.J., Smith S.G., Walters M.L., Merrick M.T., Chen J., Stevens M.R. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary Report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (2011).
成績單
The pelvic examination is performed for diagnostic, screening and treatment purposes as a part of gynecologic, obstetric and sexual health care. A comprehensive pelvic exam includes assessment of the external genitalia-which will be discussed in this video, followed by examination of the vagina and cervix with a speculum-to be covered in the video titled Pelvic Exam Part II; and a bimanual evaluation of the pelvic organs-reviewed in Part III of this series.
Here, we will first discuss how to introduce this exam to a patient. Subsequently, we will review the steps for external genitalia assessment, which includes inspection as well as digital evaluation.
Before discussing the physical examination steps, let’s review how to introduce this exam to a patient, the set-up necessary and a few general considerations. The pelvic exam can feel invasive to patients, so it is important to do everything possible to make them feel comfortable and empowered, rather than vulnerable. Right at the start you must establish an expectation of comfort and ask your patient to communicate their questions and concerns during the visit. If the patient has had a pelvic exam before, you should inquire about that experience. Reassure the patient by saying something like “Dialogue”.
Before beginning with the procedure, it is important that you introduce and summarize the exam, “Dialogue”. Remember, that while it is always important to avoid extremely clinical language, certain colloquial words can cross the line from being caring to being overly intimate during this exam. It is helpful to avoid the words “touch” and “feel,” which can feel sexualized in this context; instead, the words “assess,” “check,” “inspect,” or “examine” should be used. The words “bed” and “sheet” should be avoided, and “table” and “drape” should be used instead. Also, a clinician should use the word “footrests” rather than “stirrups”. It’s a good idea to avoid telling patients to “relax” because it’s a hard order for a patient to follow when they’re anxious. Practicing clinicians often utilize a chaperone for their own or the patient’s comfort, and based on institutional policies. However, in this video demonstration we will not be using a chaperone. Ask the patient to change into a gown and specify how they should dress-underwear off, and gown open in the back. Also provide the patient with a drape to place over their lap and step out of the room to give them privacy.
Set up all the supplies you will need, before beginning the exam. If you will be using lubricant at any point make sure to squeeze it onto a clean area before beginning, as you cannot touch the packets or bottle once you are wearing gloves. Make sure to have a trashcan, a working light, and a stool near the exam table.Give the patient a hand mirror so they can follow along with the exam and say, “Dialogue”. Pull out the footrests and ask the patient to place their feet over them. Raise the back of the exam table to 45-60° and ask the patient to sit back. This modified lithotomy position allows the patient to see the examiner and facilitates the examination, as the patient’s internal organs sink into the pelvic basin making them much easier to assess.
After the patient is comfortable, wash your hands thoroughly. Sit down on the stool near end of the exam table, and put on gloves. Then, place the back of your hand on the end of the table over the drape and ask the patient to slide down until they can feel the back of your hand. Next, ask them to extend their knees sideways. Now, using both your hands, fold the drape up toward the patient’s pubic bone. Then, request the patient to hold it in place using their free hand. Next, ask the patient to bring the mirror next to one of their knee. Place two fingers near, but not touching, the patient’s vulva and say, “Dialogue”. To put the patient at ease and avoid muscle spasm, establish a non-invasive contact first, “Dialogue”.
The structures evaluated during visual inspection include: mons pubis, which overlies the pubic symphysis, the labia majora that appear as rounded folds and are composed of adipose tissue, and more internally, the labia minora, the clitoris and the clitoral hood. Between the labia minora, there are two opening: the uretheral meatus and the vaginal opening, known as the introitus. The term perineum describes the tissue between the introitus and the anus. During the exam visually assess for the following: the pattern of hair growth, rashes, lesions, moles, masses, and discharge. Also look for potential signs of domestic violence such as scarring, burns, or bruising; signs of female genital mutilation; hemorrhoids; skin tags; fissures; and other irregularities.
To view these structures, position the index and middle fingers of dominant hand in a “peace” sign and keep the other fingers tucked. With the pads of your index and middle fingers, separate the labia minora and majora on one side to inspect the entirety of the sulcus. Keep your hand low and take care to avoid accidental extraneous contact with the clitoris by keeping fingers that aren’t being used tucked in. Using the same two fingers, separate the labia minora to view the vaginal introitus and urethral opening. Then, rotate your wrist up and use the back of the two fingers to retract the clitoral hood and view the clitoral shaft. Lastly, make a fist, and using the back of your fist pull away one buttock to view the anus. If you notice a mole or freckle, point it out to the patient and let them know they should regularly check it for changes, just as they would with moles elsewhere on their body.
The next part of the exam is the digital assessment of the vestibular glands, the vagina and the cervix. To start, first lubricate the turn your dominant index finger. Let the patient know you will be placing a finger in their vagina. In palm down position, place the lubricated finger into the vaginal introitus to just beyond your first knuckle. Then gently pinch the tissue between your thumb and the inserted finger at five and seven o’clock positions to assess the Bartholin’s glands located posteriorly. Watch the patient’s face for signs of discomfort and note if you feel any palpable masses.
Next, apply posterior pressure and rotating your palm up. Then using the thumb and middle finger separate the labia minora to visually inspect the urethral meatus and the openings of the paraurethral or Skene glands-located bilaterally next to the urethral meatus. Note the signs of inflammation and presence of discharge. Express the Skene’s glands by tapping gently upward with your index finger at one and eleven o’clock positions. If the glands are infected they discharge into the urethra, so finish by making a gentle beckoning motion at twelve o’clock to check if the glands release any discharge, which is absent in this case.
Then, release the labia and insert your finger farther to locate the cervix; assess its depth and direction. This will help you choose the correct speculum size and also help you decide where to angle the speculum during the other part of the exam.If you can easily locate the cervix while sitting down, the patient may need a short speculum. If you cannot easily locate the cervix, then you might have to stand up and the use a medium or a longer speculum.
Next, perform digital vaginal assessment. Slide your index finger halfway out and then rotate to palm down position. Subsequently, insert your middle finger by placing it over the top of your index finger and then place them side-by-side.Now, drop your wrist and pull down toward the perineum to make space above your fingers. Next, ask the patient to perform the Valsalva maneuver by bearing down as if having a bowel movement and assess cystocele, which refers to anterior bladder prolapse. Following that, lift your wrist up to apply anterior pressure toward the bladder until space underneath the fingers can be seen. Again, ask the patient to bear down while assessing for rectocele denoted by rectal herniation into the back wall of the vagina.
Next, lower your wrist so the fingers are flat and centered and gently separate them. This will also help in choosing the right speculum for the following part of this exam. If you’re having difficulty in separating your fingers, the exam should be performed with a small size speculum.Finally, assess the tone of the pubococcygeal muscle by asking the patient to squeeze around your fingers as if they are stopping the flow of urine. This maneuver is called the Kegel’s exercise. A firm squeeze represents a healthy and toned pelvic floor. Remove your fingers and discard the gloves. This completes the first part of the pelvic exam.
You’ve just watched JoVE’s video on the approach to the pelvic examination and assessment of the external genitalia. In this video, we reviewed how to introduce the pelvic exam to a patient, demonstrated the inspection of the external genitalia, and showed the steps to be performed during the digital assessment of the cervix and vagina. As always, thanks for watching!
