Maintenance of a Lateral Fluid Percussion Injury Device
Summary
Proper care and maintenance are essential for a lateral fluid percussion injury (LFPI) device to function reliably. Here, we demonstrate how to properly clean, fill, and assemble an LFPI device, and ensure that it is adequately maintained for optimal results.
Abstract
Traumatic brain injury (TBI) accounts for roughly 2.5 million emergency room visits and hospitalizations annually and is a leading cause of death and disability in children and young adults. TBI is caused by a sudden force applied to the head and, to better understand human TBI and its underlying mechanisms, experimental injury models are necessary. Lateral fluid percussion injury (LFPI) is a commonly used injury model due to similarities in the pathological changes found in human TBI compared to LFPI, including hemorrhages, vascular disruption, neurological deficits, and neuron loss. LFPI employs a pendulum and a fluid-filled cylinder, the latter having a moveable piston at one end, and a Luer lock connection to stiff, fluid-filled tubing at the other end. Preparation of the animal involves performing a craniectomy and attaching a Luer hub over the site. The next day, the tubing from the injury device is connected to the Luer hub on the animal’s skull and the pendulum is raised to a specified height and released. The impact of the pendulum with the piston generates a pressure pulse which is transmitted to the intact dura mater of the animal via the tubing and produces the experimental TBI. Proper care and maintenance are essential for the LFPI device to function reliably, as the character and severity of the injury can vary greatly depending on the condition of the device. Here, we demonstrate how to properly clean, fill, and assemble the LFPI device, and ensure that it is adequately maintained for optimal results.
Introduction
Traumatic brain injury (TBI) is caused by a sudden force applied to the head. Following primary injuries resulting from the physical impact, TBI survivors commonly experience secondary injuries, including cognitive deficits and neurological dysfunctions that are associated with physiological responses to the initial injury1. It is estimated that roughly 69 million individuals worldwide suffer from TBI annually2. In the United States alone, approximately 2.5 million TBI-related emergency room visits and hospitalizations occur each year, making TBI one of the leading causes of disability and death among children and young adults3. TBI can be classified as mild, moderate, or severe, with mild TBI (mTBI) accounting for approximately 70%-90% of TBI cases4. Histological and cognitive TBI pathology can occur within minutes to hours of injury, and the effects of TBI can persist for months to years after initial damage5.
The development of experimental models has been instrumental in understanding the effects and underlying mechanisms of TBI. One such model, the lateral fluid percussion injury (LFPI), is commonly used to assess TBI in vivo. LFPI closely reproduces pathologies associated with human TBI, including vascular disruptions, hemorrhages, neuronal loss, inflammation, gliosis, and molecular disturbances6,7,8. The LFPI technique is used for a diverse set of experimental applications, including modeling pediatric TBI, as well as chronic neurodegenerative conditions, such as chronic traumatic encephalopathy9,10. LFPI is a well-defined and reproducible method of experimental TBI that allows for the severity of the injury to be adjusted11. The LFPI device has several important components, including: a pendulum with a weighted hammer, a piston, a fluid-filled cylinder, a pressure transducer, a digital oscilloscope, and a small tube at the end of the cylinder with a Luer lock which attaches to a hub on the animal's skull (Figure 1). LFPI works by swinging the pendulum into the piston, creating a wave of pressure through the fluid (degassed deionized water or saline) into the brain of the attached animal; this increases intracranial pressure, thus replicating the mechanical features and biological changes of TBI12. Additionally, animals used in LFPI experiments undergo a craniectomy in order to expose the brain to the impact of the fluid pressure of the device.
Routine maintenance and monitoring are necessary to ensure that the LFPI device is accurately functioning. The following methods are vital in preventing the introduction of contaminating air bubbles into the device. Here, we demonstrate methods to properly clean, fill, and assemble the LFPI device. We will also discuss oscilloscope outputs and mouse righting times as ways to confirm the viability of the LFPI.
Protocol
1. Cleaning the LFPI cylinder
- Carefully detach the syringes attached to the transducer housing and fill port, as well as the cable connected to the pressure transducer (see Figure 1 for a schematic of injury device components).
- While being careful not to drop the cylinder, unscrew the hand knobs at the back of the device from the cylinder clamps to free the cylinder.
- Remove the piston at the end of the cylinder, transducer, transducer housing, and plunger O-rings.
- Drain fluid out of the cylinder.
- Add mild detergent, such as dish washing detergent, to the cylinder and scrub lightly using a dish or bottle brush13.
- To ensure that all the detergent is rinsed off, completely fill the cylinder with water and rinse thoroughly.
2. Degassing the fluid used to fill the cylinder
- Use a vacuum pump to degas the fluid before refilling the cylinder to prevent the formation of new bubbles and absorb existing bubbles.
NOTE: Approximately 1.5 L of fluid will be needed to fill the cylinder, although degassing approximately 2 L will leave a small supply for replacing any fluid lost during use and testing.
NOTE: House vacuums are too weak to effectively degas the fluid. The vacuum must be able to produce a pressure of 25-28 inHg. - Add a stir bar to the fluid and place the fluid container on a stir plate. Stirring the fluid during the degassing process helps to stimulate bubbling and the release of gas. Stirring also prevents a large sudden increase in bubbling.
NOTE: The degassing process should be over when very few bubbles are being produced; this occurs after roughly 45 min.
3. Reassembly of the LFPI device
- Apply a thin layer of petroleum jelly to the piston plunger.
- Attach the piston plunger with the plunger protruding approximately 32 mm from the cylinder14.
NOTE: Air frequently gets trapped at the plunger before the leading O-ring. To get rid of this excess air, twist the plunger while moving it in and out to work the air out of this gap. - Apply a thin layer of petroleum jelly to the other O-rings as well and attach them to the cylinder, with exception to the O-ring on the fill port.
- Wrap Teflon tape twice around the transducer's threads.
4. Refilling the LFPI device and attachment to the base
- Connect a 10 mL syringe filled with degassed fluid and free of air bubbles to the Luer lock hub on the transducer housing.
- Hold the transducer with the threaded end pointing upward, and completely fill the well inside the threaded region of the transducer with the degassed fluid using a 10 mL syringe. The goal here is to fill the transducer well without introducing any air bubbles. Be careful not to damage the delicate membrane at the bottom of the transducer well.
- With the cylinder placed at an angle to prevent air from reentering the transducer housing, attach the transducer housing to the cylinder13 and use a wrench to tighten it snugly.
- Remove the cap from the fill port and cylinder once the degassed fluid reaches approximately 2/3 of the cylinder capacity.
- Place the cylinder horizontally and finish filling the cylinder with degassed fluid.
NOTE: To avoid the formation of air bubbles, pouring the fluid in slowly is recommended14. - Replace the cap at the fill port and close all stopcocks.
- Manipulate the cylinder to work any air bubbles to the fill port14.
- Open the stopcock on the fill port and inject fluid using the syringe on the transducer housing to force any air bubbles out of the port14.
- Inspect the entire device and ensure that there are no air bubbles.
- Add a 10 mL syringe filled with degassed fluid to the Luer lock hub on the fill cap.
- Reattach the cylinder to the base using the hand screws.
- Ensure that the cylinder is horizontal and lined up with the center of the weighted hammer on the pendulum.
Representative Results
We tested the effects of air bubble contamination in an LFPI device on waveform formation. We injected air bubbles into the device and compared the oscilloscope outputs with oscilloscope data collected from a non-contaminated LFPI device. Conditions were as follows: non-contaminated, injection of 5 mL of air, injection of 10 mL of air, and injection of 15 mL of air. We kept the pendulum at a consistent height for all impacts for all conditions, and we performed 15 impacts per condition.
When performing an injury or testing the LFPI device, the pressure waveform on the oscilloscope should show a single, sharp peak (Figure 2A). The presence of air bubbles in the device will result in a waveform with several short peaks (Figure 2B), indicating bubbles that need to be removed. After reassembling the device, and before any injury session, we also recommend performing four to five test drops (no mouse attached) with the pendulum to ensure that the device is performing repeatably. In addition to irregularities in the pressure waveform, behavioral changes after injury/sham LFPI can also be indicative of whether the device is functioning properly. Injured mice should have prolonged righting reflex times after LFPI in comparison to sham mice, and these times should be monitored and recorded. Righting times that are either too long or too short may be an indication of improper device assembly and/or cleaning15. Similar symptoms can also appear gradually in a device that has been properly cleaned and filled (likely due to the slow accumulation of bubbles during routine use), indicating that it is time to repeat the cleaning and refilling. Scheduling preventive maintenance once every 6 months can help to ensure consistent performance of the LFPI device.
As seen in Table 1, the presence of air bubbles changed the voltage of the waveform when compared to a fully filled, non-contaminated LFPI device. Increasing the size of the air bubble gradually decreased the voltage of the wave, as indicated by the oscilloscope outputs.
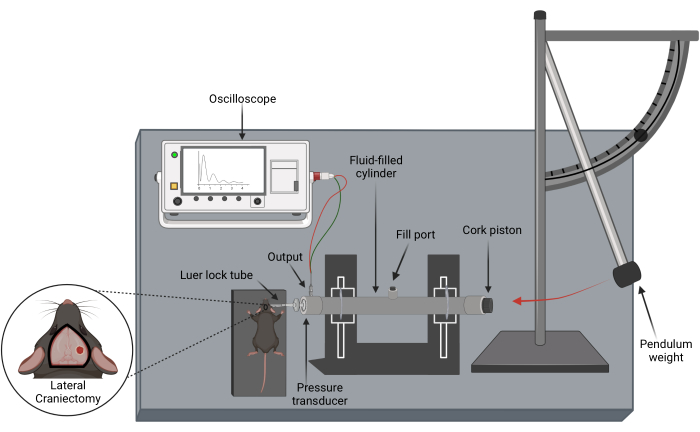
Figure 1: Schematic of the LFPI device and lateral craniectomy performed prior to injury. This device is used to reproduce TBIs with no skull fracture in animal models by causing displacement and/or deformation of the brain due to an increase in intercranial pressure. Created with Biorender.com. Please click here to view a larger version of this figure.

Figure 2: Monitoring pressure transducer output to assess LFPI device maintenance and functional status13. (A) Representative image of the pressure waveform produced by a properly cleaned and functioning LFPI device. (B) Sample image of a pressure waveform indicating the presence of air bubble contamination. Please click here to view a larger version of this figure.
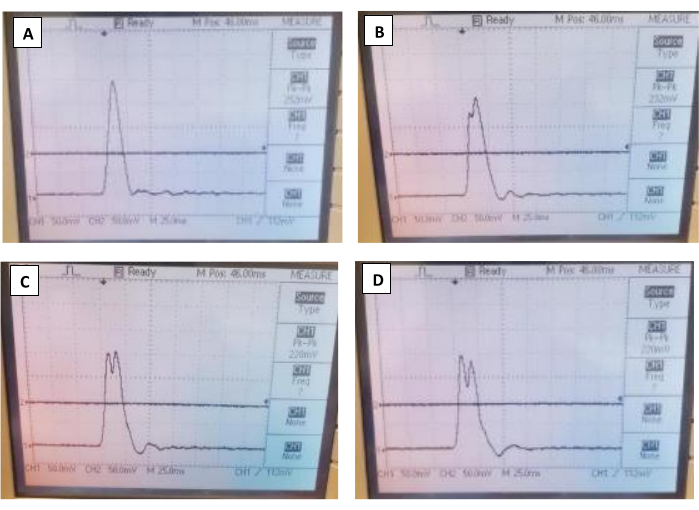
Figure 3: Representative image of oscilloscope outputs for all four conditions. (A,B,C,D) The oscilloscope outputs for the non-contaminated, 5 mL of air injection, 10 mL of air injection, and 15 mL of air injection, respectively. Please click here to view a larger version of this figure.
| Air Bubble Contamination Condition | |||||
| Filled and Non-Contaminated LFPI Device | 5 mL of Total Air Injected | 10 mL of Total Air Injected | 15 mL of Total Air Injected | ||
| Waveform Output (mV) | 240 | 218 | 230 | 218 | |
| 234 | 222 | 226 | 220 | ||
| 240 | 228 | 226 | 220 | ||
| 244 | 226 | 228 | 218 | ||
| 246 | 228 | 230 | 218 | ||
| 248 | 232 | 226 | 220 | ||
| 248 | 230 | 226 | 220 | ||
| 250 | 230 | 228 | 220 | ||
| 248 | 232 | 228 | 224 | ||
| 252 | 232 | 228 | 222 | ||
| 250 | 232 | 226 | 220 | ||
| 250 | 230 | 228 | 222 | ||
| 252 | 230 | 228 | 222 | ||
| 252 | 232 | 228 | 220 | ||
| Average Waveform Output (mV) | 246.7 | 228.7 | 227.6 | 220.3 | |
Table 1: Oscilloscope voltage outputs from non-contaminated control group compared to contaminated conditions. Paired t-tests were performed between the non-contaminated conditions and each contaminated condition. All contaminated conditions were significantly decreased when compared to non-contaminated conditions (p < 0.0001).
Discussion
The techniques outlined above demonstrate how to properly maintain an LFPI device. Routine cleaning and monitoring are necessary to keep the LFPI device functioning correctly and reliably. Additionally, due to the invasive nature of the LFPI procedure, it is imperative that the device be cleaned thoroughly to prevent infection of laboratory animals.
Avoiding the formation of air bubbles in the device is crucial for obtaining optimal injuries and pressure waveforms. Air bubbles alter the characteristics of the pressure pulse delivered to the brain, causing inconsistent injuries and making it difficult to properly reproduce clinical TBIs. The supplemental data collected here show that air bubble contamination alters the voltage of the wave produced by an impact. The oscilloscope outputs shown in Figure 3 help illustrate the effects of air on pressure waves; the waveforms are not as sharp and instead have multiple peaks when air contamination is present. The goal of the LFPI device is to provide a singular measurable fluid pulse to the brain; the results suggest that when air bubbles are present, multiple pulses are created, making it difficult to discern what pressure is being applied to the brain.
The techniques employed here reduce the likelihood of gases being introduced into the device and/or help remove any small pockets of gas that may nonetheless be contaminating the fluid. Using degassed fluid reduces the risk of air bubble contamination and can extend the maintenance interval13. Thus, the actions performed in step 2 are critical for reducing the chance of air bubble formation in the LFPI device. Steps 3.4-3.9 highlight the importance of removing lingering gases in the device prior to performing injuries. It is noteworthy that, after reassembling the injury device, visibility in both the pressure transducer and the center of the fill port is limited; thus, these areas require particular attention when checking for air bubble formation after filling the cylinder.
This procedure is specifically tailored to the LFPI device made by Custom Design & Fabrication Inc. Minor changes to the protocol may be necessary when using LFPI devices manufactured by other companies.
Cleaning and reassembling an LFPI device require time and attention, but is key to producing consistent injuries. Avoiding air bubbles is particularly important, as it can help reduce faulty results and limit the need to perform additional experiments.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors would like to thank Custom Design & Fabrication Inc. for their technical assistance and support. This work was funded by the National Institutes of Health grants R01NS120099-01A1 and R37HD059288-19.
Materials
| 2 – 10 mL syringes with Luer lock capability | Ensures that needle is secure and reduces possible leaks of fluid | ||
| Degassed fluid | Helps to reduce air bubble formation during injury procedure | ||
| Fluid Percussion Injury (FPI) device (Model 01-B) | Custom Designs & Fabrications Inc. | N/A | Injury device used to model TBI in rodents |
| Mild detergent | Allows to thoroughly clean the LFPI cylinder | ||
| Petroleum Jelly | Used as a water-repellent and protects LFPI device form rust | ||
| Teflon tape | Helps with tight seal of pipe joints on the LFPI device | ||
| *Materials other than the LFPI device can be purchased from any reliable company. |
References
- Centers for Disease Control and Prevention. Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. , (2014).
- Dewan, M. C. Estimating the global incidence of traumatic brain injury. Journal of Neurosurgery. 130 (4), 1080-1097 (2018).
- National Center for Injury Prevention and Control; Division of Unintentional Injury Prevention. . Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. , (2015).
- Holm, L., Cassidy, J. D., Carroll, L. J., Borg, J. Summary of the WHO Collaborating Centre for neurotrauma task force on mild traumatic brain injury. Journal of Rehabilitation Medicine. 37 (3), 137-141 (2005).
- Pavlovic, D., Pekic, S., Stojanovic, M., Popovic, V. Traumatic brain injury: neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary. 22 (3), 270-282 (2019).
- Dixon, C. E. A fluid percussion model of experimental brain injury in the rat. Journal of Neurosurgery. 67 (1), 110-119 (1987).
- McIntosh, T. K. Traumatic brain injury in the rat: characterization of a lateral fluid-percussion model. 神经科学. 28 (1), 233-244 (1989).
- Ma, X., Aravind, A., Pfister, B. J., Chandra, N., Haorah, J. Animal models of traumatic brain injury and assessment of injury severity. Molecular Neurobiology. 56 (8), 5332-5345 (2019).
- Nwafor, D. C. Pediatric traumatic brain injury: an update on preclinical models, clinical biomarkers, and the implications of cerebrovascular dysfunction. Journal of Central Nervous System Disease. 14, (2022).
- Turner, R. C. Modeling chronic traumatic encephalopathy: the way forward for future discovery. Frontiers in Neurology. 6, 223 (2015).
- Petersen, A., Soderstrom, M., Saha, B., Sharma, P. Animal models of traumatic brain injury: a review of pathophysiology to biomarkers and treatments. Experimental Brain Research. 239 (10), 2939-2950 (2021).
- Sullivan, H. G. Fluid-percussion model of mechanical brain injury in the cat. Journal of Neurosurgery. 45 (5), 521-534 (1976).
- Pernici, C. D. Longitudinal optical imaging technique to visualize progressive axonal damage after brain injury in mice reveals responses to different minocycline treatments. Scientific Reports. 10, 7815-78 (2020).

