Full-Endoscopic Surgery for Hypothalamic Hamartoma Resection
Özet
Hypothalamic hamartomas are rare, non-neoplastic congenital malformations mainly arising from the inferior hypothalamus or tuber cinereum. Surgical treatment is one of the most effective options, and the surgical approach must be precisely determined for each patient. Here, we describe the full-endoscopic technique for resecting hypothalamic hamartomas.
Abstract
Hypothalamic hamartomas (HH) are rare developmental anomalies of the inferior hypothalamus that often cause refractory epilepsy, including gelastic seizures. Surgical resection is an effective method to treat drug-resistant epilepsy and endocrinopathy in a suitable patient group. Open surgery, endoscopic surgery, ablative procedures, and stereotactic radiosurgery can be utilized. In this study, we aimed to describe the full-endoscopic approach for HH resection. The technique involves the use of an intraoperative ultrasonography (USG) system, a 30° rigid endoscope system that has an outside diameter of 2.7 mm with two working channels, a stylet that has an outer diameter of 3.8 mm, a monopolar coagulation electrode, a fiberoptic light guide, and the endovision system. Microforceps and monopolar electrocautery are the two main surgical instruments for HH removal. The protocol is easy to apply after a particular learning curve has been passed and shorter than open surgical approaches. It leads to less blood loss. Full-endoscopic surgery for HH is a minimally invasive technique that can be applied safely and effectively with good seizure and endocrinological outcomes. It provides low surgical site pain and early mobilization.
Introduction
Hypothalamic hamartomas (HHs) are non-neoplastic, heterotrophic tissues that contain neuronal and glial tissue in an abnormal distribution. Incidence rates of HHs are 1 in 50,000-1,000,000 people with male predominance1. HHs present different clinical symptoms, such as precocious puberty, cognitive impairment, behavioral changes, and various types of seizures, most characteristically, gelastic seizures. Mostly gelastic seizures, as well as other seizure types, are extremely refractory to antiepileptic drugs (AEDs)2,3.
Based on their morphology and relation to the hypothalamus, there are several classifications for HHs. The symptoms and the severity depend mainly on the size, location, attachment type, and degree of hypothalamic displacement. Seizures and behavioral, cognitive, and hormonal problems mostly originate from sessile HHs. Pedunculated HHs mainly cause precocious puberty4,5,6.
Seizures can be controlled surgically either by resection or disconnection of the lesion. Most favorable outcomes were obtained from near-total or total resections4. The main goal is to prevent the spreading of the epileptic burst and thus stop secondary generalized seizures. Open surgery, either pterional, transcallosal, or transventricular approach, leads to good surgical outcomes; however, the complication rate is high, up to 30%. Laser and radiofrequency thermocoagulation-based disconnection surgeries, stereotactic radiosurgery, and focused ultrasound are also described as alternatives to open surgery. The treatment approach should be selected individually since the hypothalamic area, and close structures are critical5,6,7.
The possibility that an endoscopic approach could achieve HH resection was first described in 20038. Other authors have also shown the feasibility of endoscopic resection and disconnection surgeries for HH. These studies led us to believe that, especially in sessile intrahypothalamic HHs, a full-endoscopic approach is feasible7,9,10,11. Surgical indications are mainly medically intractable gelastic seizures, neurobehavioral deterioration, and intractable endocrinopathy. Potential risk factors for surgery are mainly memory loss, endocrinopathy, behavioral and cognitive problems, and vision loss. With recent technological advancements in neuroendoscopy and surgical instruments, this study aimed to describe our technique of full-endoscopic approach for HH resection3,12,13.
CASE PRESENTATION:
A 15-year-old boy was born at term by normal vaginal delivery. The patient had first seizures 7 years ago. Perinatal history was unremarkable. First seizures were characterized by gelastic seizures; however, after 2 years, the seizures changed character, becoming tonic type. The seizure frequency was 9-10 times per day. Neurological examination revealed moderate mental retardation and no neurological deficit. From the beginning of the seizures, the patient was administered carbamazepine, valproic acid, phenobarbital, lamotrigine, levetiracetam, and clobazam in different combinations. But there was no improvement in his condition. Magnetic resonance imaging (MRI) revealed a hamartoma of the right hypothalamus. A routine scalp electroencephalography (EEG) showed active epileptogenic focus in the right frontocentral and temporal regions. During video-EEG, 10 seizures were recorded. The electrographic discharge showed a right-sided origin. Ictal and interictal single-photon emission computed tomography (SPECT) and positron emission tomography (PET) were noncontributory. Neuropsychological tests (NPT) were not performed, as the patient was not cooperative. The patient did not have endocrinological issues such as precocious puberty, and all hormonal parameters were within normal range. Since the patient had medically intractable seizures and moderate mental retardation, surgical resection of the HH was decided.
The patient did not have any complications after surgery, nor did he experience diabetes insipidus (DI) or any other endocrinopathies. The ophthalmological exam was normal, and there was no central hyperphagia or fever. The patient was discharged on postoperative Day 5. In the 25th month after surgery, he was followed up seizure-free, Engel class 1. A control MRI 2 years postoperatively showed no recurrence of the HH. The patient and his relatives stated that the patient had a better educational level and cognition; however, testing regarding neurocognition was not applied.
Protocol
The study protocol was approved by the institutional review board of Istanbul University Faculty of Medicine. Informed consent was obtained from patients for this study.
1. Preoperative procedures
NOTE: Preoperative evaluation is similar to any other medically intractable epilepsy patient. Routine scalp electroencephalography (EEG) monitoring and video-EEG monitoring, interictal and ictal single photon emission computed tomography (SPECT), magnetic resonance imaging (MRI), neuropsychological test (NPT), ophthalmological assessment with perimetry, and endocrinological assessment should be completed.
- Under general endotracheal anesthesia, place the patient supine with the head flexed on a three-pronged Mayfield head clamp.
NOTE: The patient can be placed on gel-based modifications if younger than 18 months. - Plan the incision on Kocher's point, which is 3 cm lateral to the midline and 1 cm anterior to the coronal suture. The coronal suture can be outlined by palpation.
NOTE: The entry point can be adjusted using the intraoperative ultrasonography (iUSG) system for an optimal trajectory to the HH interface and normal tissue interface. Optic or frameless electromagnetic neuronavigation systems are alternatives to iUSG for achieving proper trajectory. - Set the iUSG system with a burr-hole probe before beginning the primary surgical procedure. Most of the cases of HHs have normal-sized ventricles. The ventricle size can be seen in preoperative MRI.
- Adjust the 30° rigid endoscope system according to the surgeon's preferred position. The neuroendoscope has an outer diameter of 2.7 mm with two working channels. The sheath of the neuroendoscope has an outer diameter of 3.8 mm and a stylet.
- Set other instruments, such as a monopolar coagulation electrode, a fiberoptic light guide, and the endovision system.
- Disinfect the surgical site with swabs soaked in commercially available povidone-iodine solution at least 10x. Drape the periauricular region with sterile blankets.
- Adjust the white balance and camera clarity options. Any sterile white dressing and sterile written material can be used for the check.
2. Surgical technique
- Make an approximately 3 cm vertical skin incision on Kocher's point using a 20-number blade. After passing the skin, connective tissue, and galea, incise the periosteum. Place the automatic retractor covering the skin, subcutaneous tissue, and the periosteum to expose the bone. Enter the right ventricle since it is the nondominant hemisphere unless there is anatomical difficulty.
- Open a 14 mm diameter burr hole. The size is 14 mm due to using iUSG, which can only fit for its burr-hole probe.
- Expand the burr-hole medially or laterally according to the ultrasonographic image, visualizing the appropriate trajectory to the HH.
- Irrigate the field with isotonic saline for a clear visualization of the coronal section of the ventricles. Introduce the sheath with its stylet at the level of the foramen of Monro in coronal view.
- Remove the stylet from the sheath and then introduce the endoscope.
- Under direct visualization, advance the endoscope through the foramen of Monro. Visualize the HH protruding from the floor and the lateral wall of the third ventricle. Direct vision usually appreciates the limits of the protruding HH and the normal tissue.
- Coagulate the lesion by monopolar cautery introduced from the working channel. Remove the lesion with microforceps. Keep dissecting until the pial and arachnoid membrane are reached. Complete resection and disconnection can be confirmed by postoperative MRI.
- Achieve hemostasis by irrigation with isotonic saline solution or monopolar coagulation. Massive bleeding usually does not occur; in case of occurrence, it may necessitate leaving external ventricular drainage (EVD) or converting to open microscopic surgery.
- After hemostasis, complete the procedure by removing the endoscopic system. Suture the subcutaneous tissue with 3-0 Vicryl and the skin with 3-0 prolene.
3. Postoperative procedures and follow-up
- Begin oral intake at 6 h postoperatively. Mobilize the patients on the next day of the operation.
- Monitor the patient immediately after surgery for early complications, such as transient memory loss, weight gain, thalamic and hypothalamic infarction, diabetes insipidus, pituitary insufficiency, and visual disturbance.
NOTE: The endoscope can cause damage to the fornix, optic chiasm and tract, and hypothalamus. The monopolar cautery can cause similar destruction through the thermal effect. - Monitor the patient for intake and output balance. Ask the patient and the relatives to write down every patient's fluid intake and calculate the urine output. If the patient has pituitary insufficiency, hydrocortisone replacement therapy should be applied.
- Continue antiepileptic drugs (AED) till adequate follow-up has been established. AED can be reduced according to seizure outcome status and control electroencephalograms (EEG).
- Upon discharge, follow up the patient in the 2nd week, 1st month, 3rd month and 6th month.
Representative Results
An example of a patient treated by a full-endoscopic approach for HH resection has been presented. The preoperative MRI, intraoperative endoscopic view, and postoperative MRI have been shown in Figure 1, Figure 2, and Figure 3. There was minimal blood loss during the procedure, so it could not be measured. The procedure is short for a surgeon experienced in neuroendoscopy. For the represented case, the operation duration was 52 min. The method requires only a small incision, quick postoperative recovery, and early return to work. The patient is usually discharged on the postoperative day 1 if no complications are encountered. Because it is a resection and disconnection surgery, good seizure outcomes are accomplished in the early postoperative period.

Figure 1: Preoperative images of lesion. Preoperative T2 (A) axial, (B) sagittal, (C) coronal, (D) T2 FLAIR axial, and (E) sagittal images show an 8 x 11 x 14 mm lesion located at the inferior third ventricle protruding from the right hypothalamic region. (F) The lesion does not enhance with gadolinium administration. Please click here to view a larger version of this figure.
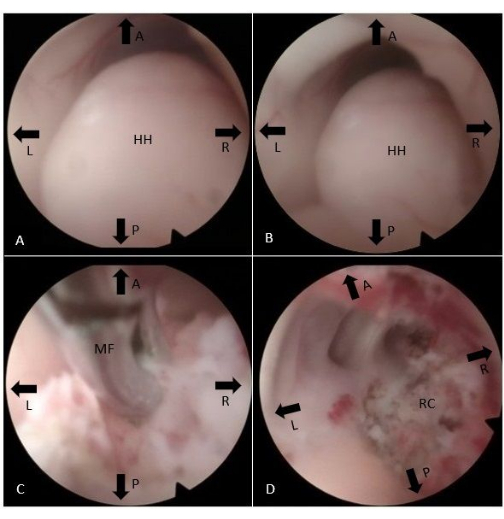
Figure 2: Endoscopic intraoperative view. (A, B) The HH bulging to the third ventricle from the right side is seen. (C) Monopolar cautery and microforceps are used to dissect and disconnect HH from the hypothalamic body. (D) The resection cavity is visualized at the end of the procedure. Abbreviations: A = Anterior, P = Posterior, L = Left, R = Right, HH = Hypothalamic hamartoma, MF = Microforceps, RC = Resection cavity. Please click here to view a larger version of this figure.

Figure 3: Postoperative images of lesion. Postoperative T2 (A) axial, (B) T2 FLAIR sagittal, and (C) coronal images show total resection and disconnection of the HH. Please click here to view a larger version of this figure.
Discussion
In 2003, Delalande classified HHs into four subtypes. Type 1 HHs are small peduncular lesions attached to the tuber cinereum, type 2 HHs are lesions protruding to the third ventricle, type 3 lesions are the combination of type 1 and type 2 HHs, and type 4 HHs are large lesions with a broad attachment to both mammillary bodies and hypothalamus and have an extension to the interpeduncular cistern8. Depending on the location of the HH, various open surgery approaches have been described. For HHs near the interpeduncular cistern, the pterional approach, and for lesions near the third ventricle, transventricular or transcallosal approaches are feasible. The complication risk increases if the lesion is attached to mammillary bodies and the tuber cinereum. Destruction of the mammillary bodies may cause neuropsychological effects, and the tuber cinereum may cause poor endocrinological outcomes12.
The pterional approach is a short and direct route to the suprasellar cistern; however, access to the third ventricle is limited, and the vicinity of the internal carotid artery and branches, optic nerve, and chiasm, third cranial nerve, and infundibulum makes surgical maneuvers more limited8,14. Due to these limitations, transventricular and transcallosal approaches are used for Delalande type 2 and 4 HHs15. However, reports showed an increased risk of memory impairment by this technique. The memory deficit is mainly attributed to forniceal injury during the transcallosal interforniceal approach and mammillary body destruction during the trans ventricular approach16,17.
Stereotactic radiosurgery by Gamma-knife is another treatment alternative for HHs. Despite the delayed action of the radiosurgery, promising results have been reported. The median number of seizures was reduced from 6.2 to 0.3. The median marginal dose was 17 Gy (13 to 26)19,20,21,22. Stereotactic laser interstitial thermotherapy (LITT) is another treatment option involving a laser probe's stereotactic placement. In the literature, it has been shown that, regardless of the HH size, stereotactic LITT reduced the morbidity compared to open surgery23,24,25. Recent studies have proposed stereoelectroencephalography (SEEG)-guided radiofrequency-thermocoagulation (RF-TC). It enables the simultaneous application of RF-TC during recording, thus providing more precise lesioning26,27.
In this technical note, the full-endoscopic approach to HHs is described. This technique is also as minimally invasive as the stereotactic approach. In addition, it does not require applying a stereotactic system and targeting by fusion with MRI. The ventricular puncture can be easily accomplished by the intraoperative USG system. It does not require preoperative preparation, and therefore, it is quick. Direct visualization of the HH is possible, and lesion resection is feasible despite laser ablation or thermocoagulation. Early seizure and endocrinological improvements are usually appreciated7,10,24. It is best suited for Delalande type 2 HHs10. Furthermore, Choi et al. described the importance of disconnection surgery in treating HHs. They showed that most intraventricular and other types of HHs are excellent candidates for endoscopic surgery. They revealed that 90% of patients had more than 50% seizure control after surgery. Despite the resected volume, disconnection is considered to be more critical. Therefore, even for larger HHs, disconnection surgery can be performed for selected cases5,28,29. However, despite its advantages, the full-endoscopic technique has limitations. It is usually not feasible for lesions that extend to the interpeduncular cistern. It bears the same risk for lesions attached to mammillary bodies and tuber cinereum11. In the postoperative period, early mobilization and return to work are possible.
In conclusion, surgical techniques should be decided according to HH's location and adjusted for each patient. The full-endoscopic resection of HH is a safe and effective approach, especially in lesions extending to the third ventricle. Disconnection should be considered in each surgery and is more important than the resection rate. Seizure and endocrinological outcomes are similar to other techniques. It is a minimally invasive technique that enables a short hospital stay and early gain of functional status.
Açıklamalar
The authors have nothing to disclose.
Acknowledgements
There is no funding source for this study.
Materials
| Burr-hole probe of intraoperative ultrasound system | Hitachi | UST-52114P | Aloka Linear UST-52114P, Frequency Range: 8 – 3 MH, Scan Angle: 90° FOV |
| Fiberoptic light guide | RiwoSpine | 806635231 | 80663523 fiber light cable Ø 3.5 mm, TL 2.3 m, 8095.09 adaptor endoscope side, 8095.07 adaptor projector side |
| Intraoperative Ultrasound system | Hitachi | Hitachi Arietta 70, Tokyo, Japan | |
| Microforceps | RiwoSpine | 89240.3023 | |
| Monopolar-coagulating electrode | RiwoSpine | 8922095000 | |
| Rigid neuroendoscope | Karl Storz | 8921092051 | 30° Hopkins pediatric telescope, outside diameter 2.7 mm |
| Sheath for the telescope | Karl Storz | 892209510 | 3.8 mm outside diameter with two working channels |
Referanslar
- Kerrigan, J. F., et al. Hypothalamic hamartoma: Neuropathology and epileptogenesis. Epilepsia. 58, 22-31 (2017).
- Gascon, G. G., Lombroso, C. T. Epileptic (Gelastic) Laughter. Epilepsia. 12, 63-76 (1971).
- Berkovic, S. F., et al. Hypothalamic hamartoma and seizures: a treatable epileptic encephalopathy. Epilepsia. 44 (7), 969-973 (2003).
- Wait, S. D., Abla, A. A., Killory, B. D., Nakaji, P., Rekate, H. L. Surgical approaches to hypothalamic hamartomas. Neurosurg Focus. 30 (2), E2 (2011).
- Choi, J. U., et al. Endoscopic disconnection for hypothalamic hamartoma with intractable seizure. Report of four cases. J Neurosurg. 100, 506-511 (2004).
- Shim, K. W., et al. Treatment modality for intractable epilepsy in hypothalamic hamartomatous lesions. Neurosurgery. 62 (4), 847-856 (2008).
- Shim, K. W., Park, E. K., Kim, D. S. Endoscopic treatment of hypothalamic hamartomas. J Korean Neurosurg Soc. 60 (3), 294-300 (2017).
- Delalande, O., Fohlen, M. Disconnecting surgical treatment of hypothalamic hamartoma in children and adults with refractory epilepsy and proposal of a new classification. Neurol Med Chir (Tokyo). 43 (2), 61-68 (2003).
- Valdueza, J. M., et al. Hypothalamic hamartomas: with special reference to gelastic epilepsy and surgery. Neurosurgery. 34 (6), 949-958 (1994).
- Chibbaro, S., et al. Pure endoscopic management of epileptogenic hypothalamic hamartomas. Neurosurg Rev. 40 (4), 647-653 (2017).
- Ng, Y. T., et al. Endoscopic resection of hypothalamic hamartomas for refractory symptomatic epilepsy. Neurology. 70, 1543-1548 (2008).
- Bourdillon, P., et al. Surgical treatment of hypothalamic hamartomas. Neurosurg Rev. 44 (2), 753-762 (2021).
- Feiz-Erfan, I., et al. Surgical strategies for approaching hypothalamic hamartomas causing gelastic seizures in the pediatric population: transventricular compared with skull base approaches. J Neurosurg. 103, 325-332 (2005).
- Dorfmüller, G., Fohlen, M., Bulteau, C., Delalande, O. Surgical disconnection of hypothalamic hamartomas. Neurochirurgie. 54, 315-319 (2008).
- Ng, Y. T., et al. Endoscopic resection of hypothalamic hamartomas for refractory symptomatic epilepsy. Neurology. 70 (17), 1543-1548 (2008).
- Rosenfeld, J. V., Freeman, J. L., Harvey, A. S. Operative technique: The anterior transcallosal transseptal interforniceal approach to the third ventricle and resection of hypothalamic hamartomas. J Clin Neurosci. 11 (7), 738-744 (2004).
- Rosenfeld, J. V., Feiz-Erfan, I. Hypothalamic hamartoma treatment: surgical resection with the transcallosal approach. Semin Pediatr Neurol. 14 (2), 88-98 (2007).
- Ng, Y. T., et al. Transcallosal resection of hypothalamic hamartoma for intractable epilepsy. Epilepsia. 47 (7), 1192-1202 (2006).
- Castinetti, F., Brue, T., Morange, I., Carron, R., Régis, J. Gamma Knife radiosurgery for hypothalamic hamartoma preserves endocrine functions. Epilepsia. 58, 72-76 (2017).
- Akai, T., Okamoto, K., Iizuka, H., Kakinuma, H., Nojima, T. Treatments of hamartoma with neuroendoscopic surgery and stereotactic radiosurgery: a case report. Minim Invasive Neurosurg. 45 (4), 235-239 (2002).
- Abla, A. A., et al. Gamma Knife surgery for hypothalamic hamartomas and epilepsy: patient selection and outcomes. J Neurosurg. 113, 207-214 (2010).
- Selch, M. T., et al. Linear accelerator stereotactic radiosurgery for the treatment of gelastic seizures due to hypothalamic hamartoma. Minim Invasive Neurosurg. 48 (5), 310-314 (2005).
- Hoppe, C., Helmstaedter, C. Laser interstitial thermotherapy (LiTT) in pediatric epilepsy surgery. Seizure. 77, 69-75 (2020).
- Calisto, A., et al. Endoscopic disconnection of hypothalamic hamartomas: safety and feasibility of robot-assisted, thulium laser-based procedures. J Neurosurg Pediatr. 14 (6), 563-572 (2014).
- Curry, D. J., Raskin, J., Ali, I., Wilfong, A. A. MR-guided laser ablation for the treatment of hypothalamic hamartomas. Epilepsy Res. 142, 131-134 (2018).
- Wei, P. H., et al. Stereoelectroencephalography-guided radiofrequency thermocoagulation for hypothalamic hamartomas: Preliminary evidence. World Neurosurg. 114, e1073-e1078 (2018).
- Bourdillon, P., et al. Stereo electroencephalography-guided radiofrequency thermocoagulation (SEEG-guided RF-TC) in drug-resistant focal epilepsy: Results from a 10-year experience. Epilepsia. 58 (1), 85-93 (2017).
- Wethe, J. V., et al. Cognitive functioning before and after surgical resection for hypothalamic hamartoma and epilepsy. Neurology. 81 (12), 1044-1050 (2013).
- Choi, J. U., Kim, D. S. Treatment modalities for intractable epilepsy in hypothalamic hamartoma. Adv Tech Stand Neurosurg. 39, 117-130 (2012).

.
