Exploración pélvica II: Examen con espéculo
English
分享
概述
Fuente:
Alexandra Duncan, GTA, Praxis clínica, New Haven, CT
Cocinero de Tiffany, GTA, Praxis clínica, New Haven, CT
Jaideep S. Talwalkar, MD, medicina interna y Pediatría, Facultad de medicina de Yale, New Haven, CT
Colocación de espéculo cómodo es una habilidad importante para los proveedores a desarrollar, ya que el espéculo es una herramienta necesaria en muchos procedimientos ginecológicos. Pacientes y los proveedores a menudo están preocupados por el examen de espéculo, pero es totalmente posible Coloque un espéculo sin malestar del paciente. Es importante para el clínico conocer el papel que desempeña el lenguaje en la creación de un ambiente confortable; por ejemplo, un proveedor debe consultar el espéculo “cuentas” en lugar de “hojas” para evitar perturbar al paciente.
Hay dos tipos de espéculos: metal y plástico (figura 1). Esta demostración utiliza plástico, espéculos de plástico son más comúnmente utilizados en las clínicas para las pruebas de rutina. Cuando se utiliza un espéculo de metal, recomienda el uso de un espéculo de Graves si el paciente ha dado a luz por vía vaginal y un espéculo Pederson si el paciente no tiene. Espéculos de Pederson y tumbas son formas diferentes, y ambos vienen en muchos tamaños diferentes (medio se utiliza más a menudo). Antes de colocar un espéculo de metal, es útil realizar un examen cervical digital para evaluar el tamaño de espéculo adecuado. La profundidad y la dirección de la cerviz se calcula colocando un dedo en la vagina. Si el cuello uterino de la paciente puede localizar mientras el paciente está sentado, es probable que el paciente tiene una vagina poco profunda y por lo tanto debe ser más cómodo con un espéculo de metal corto.

Figura 1. Una fotografía de espéculos disponibles comercialmente en diferentes tamaños.
Espéculos de plástico están en forma de Pederson espéculos de metal y vienen en diferentes tamaños. Para determinar el tamaño adecuado para un espéculo plástico, el examinador coloca dos dedos en la vagina del paciente, Palma abajo e intenta separar los dedos: Si no hay ningún espacio entre los dedos, debe utilizarse un espéculo plástico pequeño; Si hay espacio entre los dedos, debe utilizarse un medio. El examen no debe realizarse con un espéculo grande (como lo es significativamente mayor) sin antes de determinar la longitud de la vagina.
El espéculo se usa para realizar la prueba de Papanicolaou como parte de exámenes de detección del cáncer de cuello uterino. Cáncer de cuello uterino fue la principal causa de muerte por cáncer para las mujeres en los Estados Unidos, pero en las últimas décadas el número de casos y muertes ha disminuido significativamente de1. Este cambio se le atribuye el descubrimiento hecho por Georgios Papanicolaou en 1928 que el cáncer de cuello uterino podría ser diagnosticado por frotis vaginales y cervicales. La prueba de Papanicolau, como se le llama ahora, detecta las células anormales en el cuello uterino, canceroso y precanceroso. Las guías actuales para los intervalos de detección recomendadas pueden encontrarse a través de la Task Force de servicios preventivos Estados Unidos (USPSTF) sitio Web2.
La prueba puede realizarse utilizando cualquiera de los dos 1) una diapositiva de cristal convencional y fijador con un cepillo espátula y endocervical (el tradicional “citología vaginal”) o 2) más comúnmente utilizados de citología de base líquida con una escoba cervical o un cepillo espátula y endocervical (figura 2). No importa qué herramientas se utilizan, las muestras se recogen desde dentro el os externo y escamoso o zona de transición en el sistema operativo (figura 3). Este video muestra la espátula y cepillo endocervical con citología de base líquida, como la preparación de líquidos es una técnica más efectiva para la detección de lesiones cervicales, y el cepillo espátula y endocervicales mejorar la recogida de la muestra.

Figura 2. Herramientas de prueba de Papanicolaou. Se muestra en la secuencia son: un frasco de citología líquida cervical escoba, espátula y cepillo endocervical.
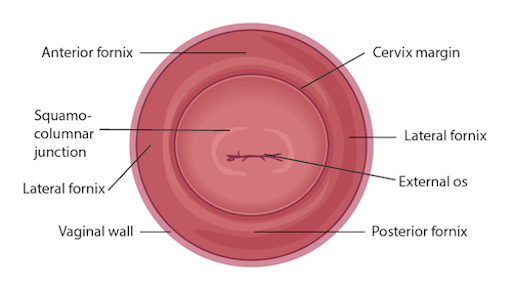
Figura 3. Diagrama de la cerviz conestructuras relevantes etiquetadas.
Procedure
Applications and Summary
This video reviewed the techniques for performing a comfortable speculum exam and collecting the samples for a Pap test. Before the exam is started, the examiner should ensure all supplies are prepared and let the patient know what to expect. Being able to perform a comfortable speculum exam is an important skill for any practitioner, as it is used in a wide variety of gynecological procedures and can provide a wealth of information. When the speculum is inserted, it is possible to observe the cervix and vaginal walls for a variety of signs including tone, color, discharge, lesions, polyps, ulcerations, and more-all of which may be clinically significant and can help with the process of diagnosis. A well-inserted speculum also allows easy access to the cervical os, at which point samples may be taken for the Pap test (as well as for other screenings, like chlamydia and gonorrhea). It's necessary to use a speculum to access the cervix for many other procedures, including inserting or removing an intrauterine device (IUD), a loop electrosurgical excision procedure (LEEP), and more.
Many patients may feel anxiety about the speculum and experience it as the most invasive part of the gynecological exam. The provider can offer the patient general support and empathy, along with specific tools to make the exam more comfortable for themselves. Asking the patient to take a deep breath and then bear down as if having a bowel movement before insertion can open the vaginal introitus and greatly aid comfort. The examiner may offer a particularly anxious patient the opportunity to insert the speculum themselves by placing it upside-down with the handle pointing toward the ceiling as the provider talks them through opening it3. It is often easier to get a clear view of the cervix with an upside-down insertion, but it is not a technique practitioners should employ, because it places the examiner's hand directly against the patient's clitoris.
There are many things the practitioner can do to ensure the exam is comfortable. The speculum should be inserted at an oblique angle to avoid putting too much direct pressure on the urethra. When the speculum is inserted fully, the bills should be angled below where the cervix was located during the digital exam. The practitioner can then apply enough posterior pressure to the speculum, so there is space visible in the vagina over the bills; this allows the bills to be opened without putting pressure on the delicate anterior structures. The most important thing is to never insert or remove a speculum while the bills are open. This is very painful and risks injuring the patient. The examiner should not touch the thumb lever until the speculum is positioned fully and ready to be opened. The lock on the speculum should be released fully before removal, and any pressure maintained manually. Once the cervix is free, the thumb lever should be completely released and the speculum smoothly removed the rest of the way, allowing the vaginal walls to close the bills on the way out.
References
- Cervical Cancer Statistics. U.S. Preventive Services Task Force. Centers for Disease Control and Prevention (2014).
- Cervical Cancer: Screening. Recommendation Summary. U.S. Preventive Services Task Force (2012).
- Wright, D., Fenwick, J., Stephenson, P., Monterosso, L. Speculum 'self-insertion': a pilot study. Journal of Clinical Nursing. 14(9): 1098-1111 (2005).
成績單
The speculum exam is used in a wide variety of gynecological procedures and can provide a wealth of diagnostic information. The speculum is a bivalve instrument, which is utilized for separating the walls of the vaginal canal. This not only allows for visual inspection of the cervix, but also provides an access to this region for specimen collection during diagnostic procedures such as the Papanicolau, or Pap test, which is performed to check for any precancerous changes. This video will illustrate the proper technique of using the speculum for cervical inspection, and the appropriate method for collection of samples for the Pap test.
Let’s begin with the review of the steps involved in prepping for the speculum exam and the Pap test, followed by a discussion of what a physician should look for while inspecting the cervix through the speculum. There are different types of commercially available specula. Some are made up of disposable plastic, while the metal ones are reusable. In this demonstration, we will use a plastic speculum.
Before starting the exam, it is essential to familiarize yourself with the instrument to be used and understand how it functions. After that you shall begin with the exam. Remember, this procedure usually comes after the external pelvic inspection, so at this point the patient history has been obtained, and they are already in the modified lithotomy position.
Make sure that the patient is seated at the end of the table to allow compete insertion of the speculum. Also lay out the supplies for the Pap test, including a cytology canister; lubricant squeezed onto a clean tray with a liner, and a spatula and endocervical brush OR just a cervical broom to collect the cell sample.Label the liquid cytology canister with the patient’s information. Then unscrew the lid of the canister until it is resting on top such that it can be easily lifted off.
It is essential to understand how to hold a speculum. In case you’re using a plastic speculum, place it in your non-dominant hand and position your index finger above the bills, your middle finger below the bills, and your thumb on the back of the speculum, avoiding the thumb lever as that would open the speculum. Using your dominant hand spread the water-based lubricant on the outside of the bills. Show the speculum to the patient without pointing it directly at them, and let them know what to expect during the exam, “Dialogue”.
Start by letting the patient know that you will first place the back of your hand on their thigh. This is done to prepare the patient for the exam by establishing a non-invasive contact first. Now separate the labia minora with the dominant index and middle finger pads to get a clear view of the vaginal introitus. Next, explain the relaxation technique to the patient, “Dialogue”. The vaginal introitus should open up as the patient bears down. Let the patient know that you are about to insert the speculum, “Dialogue” and place it halfway into the vaginal canal, keeping the bills at about 45° angle. Next, bring your non-dominant hand to the bottom handle and rotate the speculum flat, while simultaneously clearing the labia on both sides. Then angle the tip of the bills toward the floor and insert fully, such that the tip ends up below the cervix. Stop when the speculum is flushed against the patient’s pelvis.
Next place one of the dominant fingers inside the bills and apply strong posterior pressure while pulling down on the handle with the other hand until it is perpendicular to the floor. Make sure you apply enough pressure to see the space above the speculum. Now, while maintaining posterior pressure with the finger inside the speculum, you can smoothly depress the thumb lever to open the bills. Stop once resistance is met. Then engage the lock by pushing the thumb lever up one or two clicks and remove the finger from inside the speculum. Hold the speculum steady and, using a light source, check if the cervix is visible. Note the tone, color, and position of the cervix and observe for discharge, lesions, polyps, ulcerations, and masses.
You can visually inspect the lower intravaginal part of the cervix. This includes the exocervix, which is normally 2-3 cm in diameter, pink in color, and has a smooth surface; the external os, which is the opening of the endocervix into the vagina; and the four fornices, which are the recesses between the cervix margin and the vaginal wall.
After the visual inspection of the cervix, proceed to collecting samples for the Pap test. With the speculum still in place, insert the spatula into the vagina, being careful not to touch the walls. Position the spatula with its long end in the os, and the short end pressed against the junction. Now rotate it 360°, while maintaining consistent pressure and contact with the exocervix. Carefully remove the spatula avoiding the vaginal walls. Place the spatula into the open cytology canister and thoroughly rinse it by vigorous swirling in the liquid following the manufacturer’s instructions. Next, insert the endocervical brush into the vagina avoiding contact with the walls. Push the brush into the os until only the bottom bristles are exposed and then slowly rotate it 180° in one direction. Do not over rotate. Carefully remove the brush avoiding the walls, and place it into the cytology canister. Thoroughly rinse the brush by vigorous swirling and press it repeatedly against the sides of the canister to release material. Instead of using both spatula and brush, one can use just the endocervical broom, which has different sizes of bristles forming a triangular pattern. If using this, then you would insert it so the longer bristles rest in the os and the shorter rest on the transition zone and rotate it about five to ten times, depending on manufacturer’s instructions. The release of the sample is same as for that for the endocervical brush.
After sample collection is complete, release the locking mechanism by pressing down on the thumb lever, and while holding the lever down and bills open, remove the speculum about two to three inches out, to ensure that the cervix is cleared off the tip of the bills. Remove your thumb from the lever and place it on the handle. Finally, rotate the speculum by 45° while smoothly removing it all the way out. Have your hand underneath the speculum to catch any possible discharge, and discard the speculum, if disposable. At the end, replace the canister lid. Now the sample is ready for subsequent cytological analysis.
“Examiner explaining different types of specula-the similarities and differences”
You’ve just watched JoVE’s illustration of the speculum exam and the Pap test. You should now understand how to use the vaginal speculum and how to collect cervical cell sample for diagnostic evaluation. As always, thanks for watching!
