골반 시험 II: 스펙큘럼 시험
English
分享
概述
근원:
알렉산드라 던컨, GTA, 프액시스 임상, 뉴 헤이븐, CT
티파니 쿡, GTA, 프랙시스 임상, 뉴 헤이븐, CT
자이딥 S. 탈워와르, MD, 내과 및 소아과, 예일 의과 대학, 뉴 헤이븐, CT
스펙럼은 많은 부인과 절차에서 필요한 도구이기 때문에 편안한 추측 배치를 제공하는 것은 공급자가 개발하는 중요한 기술입니다. 환자와 공급자는 수시로 speculum 시험에 관하여 염려합니다, 그러나 참을성 있는 불편 없이 speculum를 놓는 것은 전적으로 가능합니다. 임상의가 편안한 환경을 조성하는 데 언어가 수행하는 역할을 인식하는 것이 중요합니다. 예를 들어 공급자는 환자를 화나게하지 않도록 “블레이드”가 아닌 “청구서”를 참조해야 합니다.
금속과 플라스틱(그림 1)의두 가지 유형이 있습니다. 이 데모는 플라스틱 스펙럼이 일상적인 테스트를 위해 클리닉에서 가장 일반적으로 사용되기 때문에 플라스틱을 활용합니다. 금속 스펙큘럼을 사용하는 경우 환자가 질을 출산한 경우 그레이브스 스펙럼을 사용하는 것이 좋습니다. 페더슨과 그레이브스 스펙럼은 모양이 다르며, 둘 다 다양한 크기로 제공됩니다 (매체는 가장 자주 사용됩니다). 금속 스펙럼을 배치하기 전에 적절한 스펙큘럼 크기를 평가하기 위해 디지털 자궁 경부 검사를 수행하는 것이 도움이됩니다. 자궁 경부의 깊이와 방향은 한 손가락을 질에 배치하여 추정됩니다. 환자의 자궁 경부가 환자가 앉아있는 동안 위치 할 수 있다면 환자가 얕은 질을 가지고 있으므로 짧은 금속 스펙룸으로 가장 편안해야합니다.

그림 1. 다양한 크기의 시판되는 스펙터클 사진.
플라스틱 스펙럼은 모두 페더슨 금속 스펙럼 모양이며 다양한 크기로 제공됩니다. 플라스틱 스펙럼에 적합한 크기를 평가하기 위해 심사관은 환자의 질에 두 손가락을 손바닥아래로 놓고 손가락을 분리하려고 시도합니다: 손가락 사이에 공간이 없다면 작은 플라스틱 스펙큘럼을 사용해야 합니다. 손가락 사이에 공간이 있는 경우 중간 을 사용해야 합니다. 시험은 먼저 질 운하의 길이를 결정하지 않고 (상당히 더 길기 때문에) 큰 관증으로 수행되어서는 안됩니다.
스펙큘럼은 자궁 경부암 검진의 일환으로 파파니콜라우 검사를 수행하는 데 사용됩니다. 자궁 경관암은 한 때 미국에 있는 여자를 위한 암 죽음의 주요한 원인이었습니다, 그러나 최근 수십 년 에서 케이스및 죽음의 수는 현저하게1을감소했습니다. 이 변경은 자궁 경관암이 질과 자궁 경관 얼룩에 의해 진단될 수 있었다는 것을 1928년에 조지오스 Papanicolaou에 의해 만들어진 발견에 기인합니다. Pap 시험은 지금 불립니다, 자궁 경부에 있는 이상한 세포를 검출합니다, 암과 전암 둘 다. 권장 심사 간격에 대한 현재 지침은 미국 예방 서비스 태스크 포스 (USPSTF) 웹 사이트2를통해 찾을 수 있습니다.
시험은 1) 기존의 유리 슬라이드를 사용하여 수행될 수 있으며 주걱 및 엔토처비알 브러시(전통적인 “Pap 얼룩”) 또는 2)를 통해 보다 일반적으로 활용되는 액체 계 세포학을 자궁경부 빗자루 또는 주걱 및 엔토처비알브러시(그림 2)로수행할 수 있다. 어떤 도구가 사용하든, 샘플은 외부 OS 와 스쿼모라컬라 접합부 또는 OS 주변의 전환영역(그림 3)에서바로 안쪽에서 수집됩니다. 이 비디오는 액체 제제가 자궁 경부 병변의 검출을 위한 보다 효과적인 기술이기 때문에 액체 기반 세포학을 가진 주걱 및 내막 브러시를 시연하고, 주걱 및 내막 브러시는 표본 수집을 향상시킵니다.

그림 2. Pap 얼룩 도구. 순차적으로 표시된 액체 세포학 캐니스터, 자궁 경부 빗자루, 주걱 및 엔토처 비알 브러시.
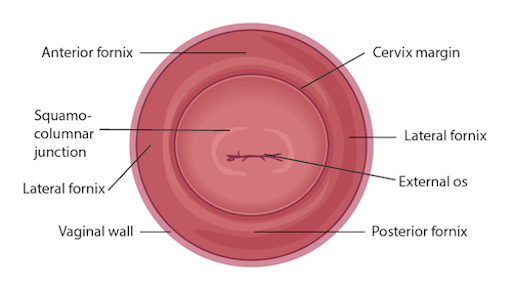
그림 3. 관련 구조가 표시된 자궁 경부의 다이어그램입니다.
Procedure
Applications and Summary
This video reviewed the techniques for performing a comfortable speculum exam and collecting the samples for a Pap test. Before the exam is started, the examiner should ensure all supplies are prepared and let the patient know what to expect. Being able to perform a comfortable speculum exam is an important skill for any practitioner, as it is used in a wide variety of gynecological procedures and can provide a wealth of information. When the speculum is inserted, it is possible to observe the cervix and vaginal walls for a variety of signs including tone, color, discharge, lesions, polyps, ulcerations, and more-all of which may be clinically significant and can help with the process of diagnosis. A well-inserted speculum also allows easy access to the cervical os, at which point samples may be taken for the Pap test (as well as for other screenings, like chlamydia and gonorrhea). It's necessary to use a speculum to access the cervix for many other procedures, including inserting or removing an intrauterine device (IUD), a loop electrosurgical excision procedure (LEEP), and more.
Many patients may feel anxiety about the speculum and experience it as the most invasive part of the gynecological exam. The provider can offer the patient general support and empathy, along with specific tools to make the exam more comfortable for themselves. Asking the patient to take a deep breath and then bear down as if having a bowel movement before insertion can open the vaginal introitus and greatly aid comfort. The examiner may offer a particularly anxious patient the opportunity to insert the speculum themselves by placing it upside-down with the handle pointing toward the ceiling as the provider talks them through opening it3. It is often easier to get a clear view of the cervix with an upside-down insertion, but it is not a technique practitioners should employ, because it places the examiner's hand directly against the patient's clitoris.
There are many things the practitioner can do to ensure the exam is comfortable. The speculum should be inserted at an oblique angle to avoid putting too much direct pressure on the urethra. When the speculum is inserted fully, the bills should be angled below where the cervix was located during the digital exam. The practitioner can then apply enough posterior pressure to the speculum, so there is space visible in the vagina over the bills; this allows the bills to be opened without putting pressure on the delicate anterior structures. The most important thing is to never insert or remove a speculum while the bills are open. This is very painful and risks injuring the patient. The examiner should not touch the thumb lever until the speculum is positioned fully and ready to be opened. The lock on the speculum should be released fully before removal, and any pressure maintained manually. Once the cervix is free, the thumb lever should be completely released and the speculum smoothly removed the rest of the way, allowing the vaginal walls to close the bills on the way out.
References
- Cervical Cancer Statistics. U.S. Preventive Services Task Force. Centers for Disease Control and Prevention (2014).
- Cervical Cancer: Screening. Recommendation Summary. U.S. Preventive Services Task Force (2012).
- Wright, D., Fenwick, J., Stephenson, P., Monterosso, L. Speculum 'self-insertion': a pilot study. Journal of Clinical Nursing. 14(9): 1098-1111 (2005).
成績單
The speculum exam is used in a wide variety of gynecological procedures and can provide a wealth of diagnostic information. The speculum is a bivalve instrument, which is utilized for separating the walls of the vaginal canal. This not only allows for visual inspection of the cervix, but also provides an access to this region for specimen collection during diagnostic procedures such as the Papanicolau, or Pap test, which is performed to check for any precancerous changes. This video will illustrate the proper technique of using the speculum for cervical inspection, and the appropriate method for collection of samples for the Pap test.
Let’s begin with the review of the steps involved in prepping for the speculum exam and the Pap test, followed by a discussion of what a physician should look for while inspecting the cervix through the speculum. There are different types of commercially available specula. Some are made up of disposable plastic, while the metal ones are reusable. In this demonstration, we will use a plastic speculum.
Before starting the exam, it is essential to familiarize yourself with the instrument to be used and understand how it functions. After that you shall begin with the exam. Remember, this procedure usually comes after the external pelvic inspection, so at this point the patient history has been obtained, and they are already in the modified lithotomy position.
Make sure that the patient is seated at the end of the table to allow compete insertion of the speculum. Also lay out the supplies for the Pap test, including a cytology canister; lubricant squeezed onto a clean tray with a liner, and a spatula and endocervical brush OR just a cervical broom to collect the cell sample.Label the liquid cytology canister with the patient’s information. Then unscrew the lid of the canister until it is resting on top such that it can be easily lifted off.
It is essential to understand how to hold a speculum. In case you’re using a plastic speculum, place it in your non-dominant hand and position your index finger above the bills, your middle finger below the bills, and your thumb on the back of the speculum, avoiding the thumb lever as that would open the speculum. Using your dominant hand spread the water-based lubricant on the outside of the bills. Show the speculum to the patient without pointing it directly at them, and let them know what to expect during the exam, “Dialogue”.
Start by letting the patient know that you will first place the back of your hand on their thigh. This is done to prepare the patient for the exam by establishing a non-invasive contact first. Now separate the labia minora with the dominant index and middle finger pads to get a clear view of the vaginal introitus. Next, explain the relaxation technique to the patient, “Dialogue”. The vaginal introitus should open up as the patient bears down. Let the patient know that you are about to insert the speculum, “Dialogue” and place it halfway into the vaginal canal, keeping the bills at about 45° angle. Next, bring your non-dominant hand to the bottom handle and rotate the speculum flat, while simultaneously clearing the labia on both sides. Then angle the tip of the bills toward the floor and insert fully, such that the tip ends up below the cervix. Stop when the speculum is flushed against the patient’s pelvis.
Next place one of the dominant fingers inside the bills and apply strong posterior pressure while pulling down on the handle with the other hand until it is perpendicular to the floor. Make sure you apply enough pressure to see the space above the speculum. Now, while maintaining posterior pressure with the finger inside the speculum, you can smoothly depress the thumb lever to open the bills. Stop once resistance is met. Then engage the lock by pushing the thumb lever up one or two clicks and remove the finger from inside the speculum. Hold the speculum steady and, using a light source, check if the cervix is visible. Note the tone, color, and position of the cervix and observe for discharge, lesions, polyps, ulcerations, and masses.
You can visually inspect the lower intravaginal part of the cervix. This includes the exocervix, which is normally 2-3 cm in diameter, pink in color, and has a smooth surface; the external os, which is the opening of the endocervix into the vagina; and the four fornices, which are the recesses between the cervix margin and the vaginal wall.
After the visual inspection of the cervix, proceed to collecting samples for the Pap test. With the speculum still in place, insert the spatula into the vagina, being careful not to touch the walls. Position the spatula with its long end in the os, and the short end pressed against the junction. Now rotate it 360°, while maintaining consistent pressure and contact with the exocervix. Carefully remove the spatula avoiding the vaginal walls. Place the spatula into the open cytology canister and thoroughly rinse it by vigorous swirling in the liquid following the manufacturer’s instructions. Next, insert the endocervical brush into the vagina avoiding contact with the walls. Push the brush into the os until only the bottom bristles are exposed and then slowly rotate it 180° in one direction. Do not over rotate. Carefully remove the brush avoiding the walls, and place it into the cytology canister. Thoroughly rinse the brush by vigorous swirling and press it repeatedly against the sides of the canister to release material. Instead of using both spatula and brush, one can use just the endocervical broom, which has different sizes of bristles forming a triangular pattern. If using this, then you would insert it so the longer bristles rest in the os and the shorter rest on the transition zone and rotate it about five to ten times, depending on manufacturer’s instructions. The release of the sample is same as for that for the endocervical brush.
After sample collection is complete, release the locking mechanism by pressing down on the thumb lever, and while holding the lever down and bills open, remove the speculum about two to three inches out, to ensure that the cervix is cleared off the tip of the bills. Remove your thumb from the lever and place it on the handle. Finally, rotate the speculum by 45° while smoothly removing it all the way out. Have your hand underneath the speculum to catch any possible discharge, and discard the speculum, if disposable. At the end, replace the canister lid. Now the sample is ready for subsequent cytological analysis.
“Examiner explaining different types of specula-the similarities and differences”
You’ve just watched JoVE’s illustration of the speculum exam and the Pap test. You should now understand how to use the vaginal speculum and how to collect cervical cell sample for diagnostic evaluation. As always, thanks for watching!
