Electrically Evoked Stapedius Reflex Measurements in Cochlear Implantation and Its Application in the Postoperative Fitting Process
Summary
The present protocol describes the measurement of the electrically evoked stapedius reflex (eSR) via cochlear implant (CI). Two applications are discussed: intraoperative detection of eSR for verification of the coupling between the cochlear implant and the auditory nerve and postoperative measurement of eSR thresholds (eSRT) for CI fitting.
Abstract
Measuring the electrically evoked stapedius reflex during the fitting of cochlear implants (CIs) provides a reliable estimation of maximum comfort levels, resulting in the programming of the CI with high hearing comfort and good speech understanding. Detection of the stapedius reflex and the required stimulation level on each implant channel is already being performed during surgery, whereby intraoperative stapedius reflexes are observed through the surgical microscope. Intraoperative stapedius reflex detection is both an indicator that the auditory nerve is responding to electrical stimulation up to the brainstem and a test for the ability to perform postoperative stapedius reflex measurements. Postoperative stapedius reflex thresholds can be used to estimate upper stimulation levels in the CI fitting process. In particular, in children or patients unable to provide feedback on loudness perception, this method avoids inadequate stimulation with the CI, which can result in poor hearing performance. In addition, overstimulation can be avoided, which could even lead to refusal to use the device.
Introduction
Electrically evoked stapedius reflex (eSRT) measurements are a known tool for verifying the coupling between a cochlear implant (CI) and the auditory nerve during surgery and postoperatively for adjusting the stimulation levels of CI programming. Whereas intraoperative measurements of the electrically evoked stapedius reflex (eSR) are quite common in clinical routine, postoperative measurements of the eSRT are still scarcely used in CI fitting because of the additional need for an acoustic impedance measurement device. However, the performance in speech perception of patients fitted with the eSRT method appears to be as good as with the method of loudness scaling1 In the latter procedure, the lower and upper limits of electrical stimulation with a CI are estimated by subjective scaling of the perceived loudness in response to stimulation on each single channel of the CI. Subjective loudness scaling requires the cooperation of the patients, who need to give feedback on their perception of electrical stimulation. Particularly young children, who today can be supplied with a CI at the age of less than one year, are not able to provide feedback on electrical stimulation. In this case, the objective eSR method is superior, and corresponding CI fitting in children allows for proper speech acquisition and cognitive development of the child at an early stage2.
The eSR method dates to the pioneering works of Stephan et al.3 who found a relation between the subjective loudness perception and the stapedius reflex threshold elicited through electrical stimulation. In these studies, a procedure was invented to measure the stapedius reflex in response to electrical stimulation in the ear canal using an acoustic impedance meter4. The correlation between the eSRT and subjective loudness ratings found originally by Stephan et al. was confirmed by other studies over the years2,4,5,6,7. Overall, programming of CIs based on eSRT results in good speech recognition scores in most patients supplied with CIs.
Today, the measurement of the eSR is a reliable tool to verify the coupling of a CI to the auditory nerve during surgery as well as a reliable estimator for upper stimulation levels in the postoperative fitting process of CIs. This paper presents both: first, a description of the eSR method during surgery for intraoperative verification that stimulation of the auditory nerve via CI is possible and processed up to the brainstem, and second, the application of the eSRT method for fitting of CIs in children and adults.
For the postoperative application of eSR testing, an acoustic impedance meter triggered by the programming interface of the CI is used to measure the eSRT during the fitting session. The entire process of CI fitting in clinical routine using the eSRT method is described. Issues to be considered such as distortions due to breathing noises or artifacts due to patient movements, which may result in distortions of the impedance measurement, are discussed. The protocol described is particularly suitable for CI fitting in children and in multiply handicapped patients.
Protocol
The procedure was approved for use in clinical routine in our department. All patients included in the report gave written consent regarding use of data and video production.
1. Intraoperative measurements of the electrically evoked stapedius reflex
NOTE: The measurement of the eSR during cochlear implantation is performed immediately after insertion of the electrode array into the cochlea. After this critical step, stimulation of the auditory nerve is possible as well as checks of the functioning of all internal CI components.
- Initial preparation
- Ensure that the surgical drapes are not too thick at the site of the implant coil, which could cause weak coupling of the test coil to the implant.
- Ensure an adequate anesthesia protocol enabling muscle contraction during the time of eSR measurement. Pay special attention to ensure that no drug-induced relaxation is effective at the time of measurement.
- Check patient data, add it to the software of the CI manufacturer (see Table of Materials), and perform in-package tests on the implant as suggested by the manufacturer.
- Check the parameter setting for intraoperative eSR measurements in the software. Set the single burst duration 到 500 ms and the minimum pulse width 到 30-40 µs. Check the guidelines of the CI manufacturer for the maximum allowed intraoperative stimulation levels.
- Measurement preparation
- After insertion of the CI electrode array into the cochlea, place the measurement coil of the CI manufacturer in a sterile packaging provided by the surgical assistant.
- Check the coupling between the measurement coil and the implant using the coupling tool of the software, while the surgeon places the measurement coil on the patient's skin over the implant housing where the receiver coil is located.
- Perform a telemetric electrical impedance measurement by clicking on the program tab 'IFT' of the software to verify the proper functioning of the implant and to measure the electrical impedances of all CI electrodes.
- In case of high impedances on many electrodes, check the CI ground electrode for skin contact and repeat the telemetry test.
- Make sure that the speaker of the facial nerve monitoring system is on. This provides the surgeon with acoustic feedback of the electrical stimulation.
- Intraoperative eSR detection
- Start the eSRT program by clicking on the program tab 'ESRT' in the software.
- Select an electrode with regular electrical impedance in the ESRT program and start stimulation with moderate stimulation values (10 charge units) while the surgeon observes the stapes tendon under the operating microscope.
- Deliver single stimuli with a burst duration of approximately 500 ms (pulse duration of 30-40 µs) and watch if any movement of the stapedial tendon is observed.
- In case no movement is detected, increase the stimulation intensity by 15% and repeat the stimulation.
- Stop increasing stimulation as soon as movement of the stapedial tendon is visible under the microscope or the maximum-allowed stimulation intensity (according to the manual) is reached.
- Repeat steps 1.3.2-1.3.5 for all electrodes with regular electrical impedance.
NOTE: For electrodes with high impedance, the effective current flow may be too small to elicit the eSR. Therefore, no eSR measurement is performed on these electrodes. In many cases, high electrode impedances decrease within the first 10 min after implantation, during eSR measurements. Telemetry measurement can be carried out again to check whether eSR detection is also possible on these electrodes.
- Interpretation of results
- Look for the eSR: if detected, it is proven that the CI electrode array is positioned in the cochlea and electrical stimulation is processed along the auditory pathway up to the brainstem.
- In case eSR detection fails, the correct placement of the CI electrode array has not been verified. Verify the correct placement by intraoperative imaging or through electrical auditory brainstem response (eABR) measurements, the latter also demonstrating the processing of the electrical stimulation up to the brainstem.
2. Postoperative determination of the electrically evoked stapedius reflex threshold levels
- Pre-planning of eSRT testing
- Perform the eSR measurement only in patients who are accustomed to electrical stimulation, at least 3-4 weeks after the activation of the CI and daily use since then.
- Review patient records for the middle ear status of both ears and surgical details of CI implantation. Exclude patients without an intact ossicular chain in both middle ears from postoperative eSRT testing.
- Discuss the procedure with the patients and, in the case of children, with their parents or accompanying persons. Plan the measurement according to the patient's needs and in a comfortable setting. Decide how to carry out the eSRT measurement: during natural sleep (for young children) or while awake. If possible, schedule measurements in very young children during nap time.
NOTE: The acoustic impedance measurement, which is performed simultaneously with the electrical stimulation, is sensitive to distortions. Therefore, the patient must stay calm during the entire procedure for about 10-30 min.
- Medical examinations before performing eSRT testing
- Arrange for a medical examination of both ears by an ENT specialist for the assessment of the ear status.
- Perform tympanometry to verify a normal middle ear status with a regular compliance maximum at ambient (zero) pressure (type A tympanogram).
NOTE: Negative pressure in the tympanic cavity (type C tympanogram) can strongly influence the detection accuracy of the eSRT. This condition often occurs in children due to a dysfunction of the Eustachian tube and a retracted eardrum. In some cases, this can be treated by the use of decongestant nasal drops. No detection of eSRT is possible with a flat type B tympanogram. - Determine if and on which ear eSRT measurements are feasible according to ear status (step 2.1.2) and select the ear with better compliance in tympanometry (step 2.2.2) for ESR detection.
- Preparation of the patient
- Check the integrity of the patient's audio processor (e.g., loose contacts, mechanical damage, or dirty microphone openings) to avoid technical problems that prevent reliable stimulation of the cochlear implant, and therefore, accurate measurement of eSRT.
- Perform telemetric electrical impedance measurements of CI electrodes (see step 1.2.3) using equipment and software (program tab IFT) provided by the implant manufacturer. Open and check the last individual CI programming used by the patient in the CI fitting software.
- Wait until the patient has fallen asleep or ensure a comfortable sitting position for measurements taken while awake. With older children, make sure that their feet are comfortably rested (e.g. using an adjustable chair) and that they are distracted during the measurement (e.g., by reading a book or watching a video [preferably without sound]).
- Place the audio processor and its coil in the proper position and check coupling with the patient's implant.
- Select the most suitable ear according to ear status and tympanometry (step 2.2.3). Place the ear probe of the acoustic impedance meter in the ear canal of the patient using a single-use ear tip. Ensure a proper fit of the probe.
- Fasten the probe cable to reduce acoustic interference: for measurements while awake fix the cable preferably to the patient's head (e.g., to a headband with two cable clips). This allows the probe cable to follow the movements of the head (Figure 1).
NOTE: In the present case, a digital version of an impedance meter based on the works of Stephan8 was used, which was equipped with a standardized ear probe. In general, any impedance meter can be used providing it accepts a trigger input of the implant interface box upon initiating an electrical stimulation burst. In contrast to using the reflex decay mode of a clinical impedance meter to register the electrical stapedius reflex, the visibility of the stapedius reflex is greatly enhanced if the impedance measurement is synchronized to the onset of electrical stimulation. - Start the software for CI fitting in normal fitting mode as during a standard subjective fitting session. Load the programming of the CI currently in use by the patient.
- Check the setting of the stimulation parameters. Use electrical stimulation bursts of at least 300 – 500 ms duration, followed by a pause of 700 ms.
NOTE: The duration of the stimulation burst affects eSRT9.
- Procedure for obtaining electrical stapedius reflex thresholds
NOTE: Always observe the patient during stimulation to avoid overstimulation or discomfort. The measurement of eSRT levels in infants or multiply handicapped persons should preferably be performed by an audiologist together with a speech therapist who is familiar with behavioral audiometry. The speech therapist is in charge of observing the patient throughout the fitting session and can provide immediate feedback if non-auditory side effects such as facial movements or eye blinking etc. occur. In older children fitting with eSRT can be performed by one CI expert, while for young children, support from a speech therapist is definitely recommended.- Select an electrode for stimulation in the middle of the electrode array and start stimulation at a moderate loudness level. If an eSR is detected by a change in acoustic impedance in response to the stimulation, reduce the stimulation level.
- Gradually increase the stimulation level in 3% steps of the actual stimulation charge until a change is detected in acoustic impedance. Carefully observe the patient to avoid uncomfortable loudness.
NOTE: With higher stimulation charges, the pulse width may be increased, which enhances the probability of triggering the electrical stapedius reflex. Set the pulse duration to a high enough value to prevent this. In a repetitive procedure (i.e., a sweep of stimulation along the electrode array), the electrical stapedius reflex will trigger at slightly lower stimulation levels than through single-channel stimulation with a longer pause in between. - Carry out the stimulation in phases in which distortions caused by breathing noises, swallowing, and patient movements are minimal.
NOTE: The heart rate of a patient may be visible as an artificial change of the acoustic impedance, which can be misinterpreted as a stapedius reflex. - As soon as the eSR is observed for the first time, increase the stimulation intensity by a further 3% step and then reduce it repeatedly until the eSR is no longer detected. An example of such a stimulation sequence and the recorded acoustic impedance changes interpreted as eSR is shown in Figure 2.
NOTE: The morphology of the acoustic impedance change caused by the stapedius reflex may significantly differ in patients with CI compared to normal hearing listeners. Both an increase or a decrease of the acoustic impedance may be observed, as well as a positive deflection of the impedance response followed by a drop to negative impedance values. The morphology itself has no effect on the estimation of the eSRT levels, but it should be verified that the impedance change occurs strictly correlated with the stimulation. - Note the lowest stimulation levels in the increasing sequence as well as in the decreasing sequence that cause triggering of the eSR. Repeat this procedure of crossing the eSRT 3x to prove the repeatability of reflex triggering. The median value of the levels noted is defined as eSRT.
NOTE: When using this up-down stimulation sequence, the values of eSRT in the ascending sequence may differ slightly from those in the descending sequence as activation of eSR will be influenced by both adaptation as well as facilitation effects of the auditory nerve. Therefore, the repetitive measurement of eSRT is recommended to avoid stimulation bias. - Repeat steps 2.4.1-2.4.5 for all electrodes of the CI.
- Activating the audio processor
- Use the eSRT levels of each electrode determined in step 2.4 to set the maximum comfort levels of the CI programming.
- Compare the eSRT-based comfort levels of the new CI programming with those used in the previous programming and determine the maximum relative change in stimulation values.
- In case of a large increase in stimulation levels, carefully activate the audio processor in microphone mode at a low volume setting according to the relative change, and gradually increase the volume up to a comfortable loudness. In case of a large decrease in these values, if some patients perceive the new programming as too soft immediately after activation, advise those patients to test the new programming at least for 1 day, as patients often become accustomed to the lower stimulation levels without any reduction in word recognition performance despite softer stimulation.
- Store multiple CI programmings with increasing volume on the audio processor. Start with programming with stimulation values to which the patient has already become accustomed and instruct the patient to switch to programming with slightly higher volume after an acclimation phase of 5-7 days as long as the auditory perceptions are not uncomfortable.
NOTE: This procedure is mainly used in young children in the initial phase of eSRT fitting to avoid the refusal of the audio processor.

Figure 1: A possible fixation option for ipsilateral positioning of the ear probe and the audio processor using a headband. The advantage of this positioning is that the probe follows head movements, which generates less distortion during the eSRT measurement than a fixation of the probe on the patient's shoulder. Abbreviations: eSR = electrically evoked stapedius reflex; eSRT = eSR thresholds. Please click here to view a larger version of this figure.
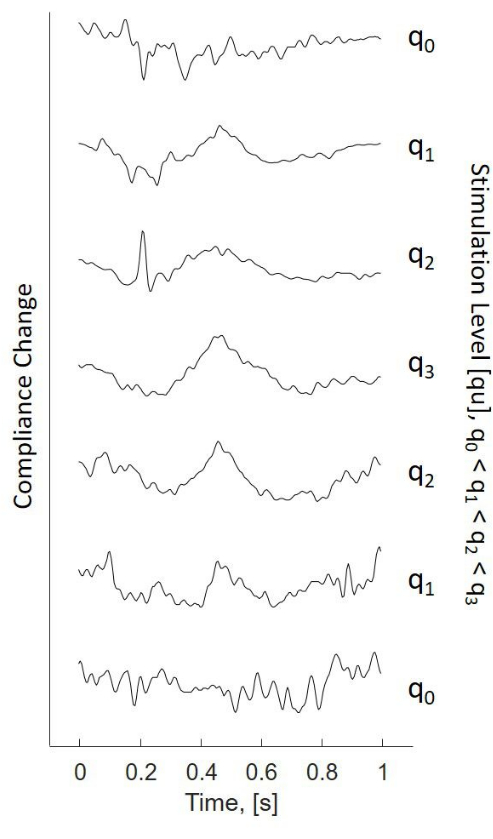
Figure 2: Compliance change due to ESR in a stimulation sequence using the up-down stimulation procedure (bottom to top starting at low stimulation levels q0). Increasing stimulation levels q0 to q3, decreasing stimulation levels q3 to q0. Single traces correspond to impedance changes observed due to triggering the eSR. Stimuli used: bursts of 300 ms, stimulation starts at time = 0. Abbreviation: eSR = electrically evoked stapedius reflex. Please click here to view a larger version of this figure.
Representative Results
Generally, the spontaneous acceptance of an eSRT-based fitting is high. In terms of audiological performance, patients with programming based on eSRT do not show significant differences in aided thresholds or word recognition scores compared to experienced patients with programming based on subjective loudness scaling3. However, such results can only be expected when reliable loudness scaling is possible.
In particular, bilateral cochlear implant users appear to benefit from eSRT-based programming. These patients often achieve similar aided hearing thresholds on both ears, as shown in Figure 3. The latter indicates that symmetry in hearing is high when using the eSRT method for fitting both implants.
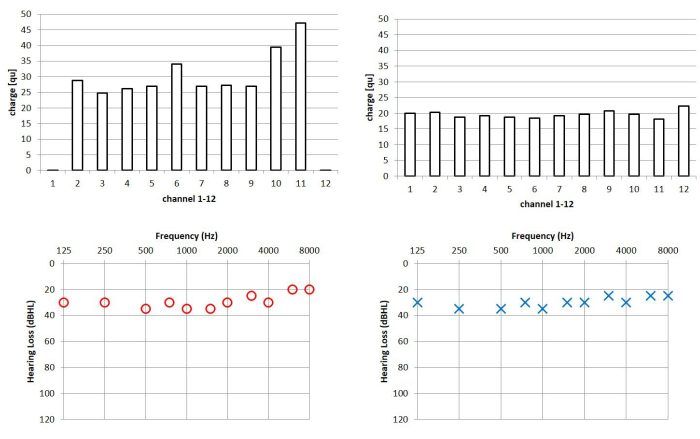
Figure 3: Case example of a bilaterally implanted patient. Upper panel: Programmed stimulation levels for the left and right cochlear implants based on the eSRT method. Zero charge indicates inactive electrodes, which are typically deactivated in case of non-auditory side effects or no auditory perceptions on particular electrodes. Lower panel: corresponding aided hearing thresholds in both ears. NOTE: While comfort levels based on eSRT are significantly different in both ears in this patient, the associated aided hearing thresholds show a high degree of symmetry. Abbreviations: eSR = electrically evoked stapedius reflex; eSRT = eSR thresholds. Please click here to view a larger version of this figure.
Patients supplied with CIs bilaterally, which were programmed using channel-specific eSRT values as comfort levels, often show scores significantly better than chance levels in binaural listening tests. In particular, children who have grown up with bilateral CIs and have acquired speech by CI reach high scores in speech in noise as well as in sound localization tests10. One requirement for good sound localization is a balanced loudness perception with the CIs, particularly in bilateral users. This criterion seems to be a priori met in bilateral CI users with CI programs based on eSRT. In the case example in Figure 3, the aided hearing thresholds on the left and right sides are almost symmetrical whereas the eSRT-based stimulation levels show a large asymmetry between left and right ears. Regarding sound localization, such patients do not show a bias in their sound localization results. An example of such a patient is shown in Figure 4, who was tested using a clinical sound localization setup consisting of five loudspeakers in the frontal hemisphere.
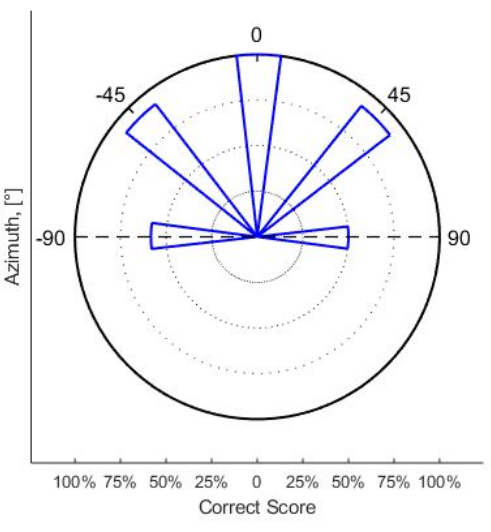
Figure 4: Angle-dependent percentages of correct scores of sound localization in a young adult bilateral patient with CI. CI programming was performed from childhood using the eSRT method. Abbreviations: eSR = electrically evoked stapedius reflex; eSRT = eSR thresholds. Please click here to view a larger version of this figure.
Apart from the high percentage of correct localizations of broadband acoustic stimuli 90% or more at angles of 0° and ±45° the symmetry was almost perfect, indicating that this patient showed no bias in the sound localization results. Therefore, loudness perception in this patient was well balanced between the left and the right CIs.
When CIs are programmed using the eSRT method, the behavior of the stapedius reflex mechanism appears to be similar to that of normal hearing listeners. In a recent study by Franke-Trieger et al.11, the stapedius reflex behavior was investigated in a free sound field. Thereby, the stapedius reflex was measured in patients with CIs who were presented with acoustic stimuli at higher sound levels via loudspeakers. In patients who were using CI programming based on the eSRT method, the sound levels at which the stapedius reflex was triggered were similar to those of normal hearing listeners11,12.
Discussion
The eSR measurement in hearing rehabilitation with CIs has two applications: first, to verify the coupling of stimulation electrodes to the auditory nerve during implantation, and second, to estimate upper stimulation levels in the postoperative programming of the audio processor.
Intraoperative measurements have the purpose of detecting the eSR as an indicator for a neural response and the processing of the electrical stimulation up to the brainstem. The contraction of the stapes tendon in response to electrical stimulation is observed visually, which requires a good view of the stapes and normal anatomical structures.
These values cannot be used for adjusting the stimulation parameters of the implant in the postoperative fitting due to the low correlation of intraoperative eSRT with postoperative loudness perception5. Intraoperative eSR measurements may further be influenced by general anesthesia13 as well as other physiological parameters (e.g., bleeding, malformation, or scar tissue).
For the detection of the eSR, an acoustic impedance measurement device is used to continuously monitor the change in acoustic impedance of the ear during electrical stimulation. To allow easy and reliable detection of the eSR, the impedance measurement should have a trigger function that is activated when the stimulus is delivered via the CI. This allows synchronous recording of eSR in response to the electrical stimulus. Alternatively, the impedance meter can be operated in continuous mode, but this appears less suitable and convenient for the application of the method. The impedance meter and the associated ear probe are typically calibrated according to audiometric standards, with the probe tone frequency of 226 Hz and sound level of 85 dB SPL. Alternatively higher frequencies can be used as probe tones as well.
The first postoperative eSRT measurement is preferentially performed 1 month after the activation of the CI. The activation session is usually scheduled 4 weeks after cochlear implantation, whereby the primary focus of the CI fitting is to make the patient accustomed to electrical stimulation at moderate stimulation levels and to motivate the patient to accept wearing the audio processor for a whole day of listening. In the next update session, which is normally scheduled 7-10 days later, the stimulation is further increased but not up to maximum comfort levels. From the third fitting session onward, the eSRT method is applicable. The perceived loudness at the eSRT is described as loud or very loud by most patients. Hence, stimulation at uncomfortable loudness levels must be avoided. Therefore, the patient needs to be carefully observed during the eSRT measurement, as eSRT may eventually be elicited but not detected. If no eSRT can be detected in both ears, the measurement must be aborted.
The method of eSRT-based programming of CIs is applicable in children as well as in adults. However, since children are typically unable to give feedback on the sound of electrical stimulation through the CI, the objective eSRT method is preferred to psychoacoustic methods, which rely on subjective feedback from the patient. It is well established by several authors that eSRT is a good estimator for comfort levels needed for programming the audio processor. This channel-specific profile created by the eSRT measurement is unique in each patient and may change over time of implant use. Therefore, the fitting of the CI must be updated at regular intervals.
The eSRT method for fitting CI certainly has one important limitation, which is the requirement of an intact middle ear. Surgical details particularly about the ossicles must be retrieved from the patient's records. Thus, postoperative eSRT measurements require preservation of the middle ear structures during surgery. In particular, during complex surgeries in case of middle ear malformations or other middle ear pathologies, the ossicular chain could be damaged. In this case, no postoperative eSRT measurement is possible on the operated ear. However, as an alternative, the ear probe can be placed on the contralateral ear and the eSRT measurement performed. In contrast to its detection, the threshold itself at which the stapedius reflex is elicited by electric stimulation does not depend significantly on the ear on which the acoustic impedance measurement is performed.
Typically, the impedance probe is placed ipsilaterally, with stimulation via the CI and reflex detection taking place in the same ear. On the ipsilateral side, the majority of the patients with CIs do not have acoustic hearing, so the probe tone of 226 Hz presented at a sound level of 85 dB SPL is not perceived. As the eSRT measurement on all channels of the CI can take a while, it is more comfortable not to hear the probe tone during the fitting procedure. If patients have acoustic hearing in the contralateral ear, the measurement may be somewhat inconvenient due to the increased listening effort during the presentation of the probe tone.
Prior to any eSRT measurement session, the current middle ear status must be checked. One limitation of eSRT-based CI fitting in children is the frequent occurrence of negative pressure in the tympanic cavity due to tube ventilation dysfunction. In this case, the acoustic impedance measurement for eSR detection is more complex. In these children, the application of nasal drops is often sufficient to relieve the pressure in the tympanic cavity to a sufficient degree that enables a successful impedance measurement in CI fitting.
The measurement of eSRT levels on all electrodes of a CI may take a while. With the equipment used in this work, a complete measurement series on 12 electrodes takes approximately 10-30 min. During this time, the acoustic impedance measurement must be stable. To ensure this condition for the entire duration of the measurement, proper positioning of the ear probe and passive cooperation by the patient are crucial.
The acoustic impedance measurement may continuously be influenced by noise from breathing and must be carefully observed as this effect may cause artifacts in ESR traces. The electrical stimulation bursts for eliciting the stapedius reflex should be initiated during phases where such distortions are small. Furthermore, the heart rate of a patient may cause a periodic change of the acoustic impedance, which can potentially be misinterpreted as a stapedius reflex.
The protocol described has been used successfully in numerous CI fitting sessions in our department and should encourage other colleagues to consider CI fitting based on eSRT in children and in multiply handicapped patients who cannot give reliable feedback on auditory perception.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors thank the cochlear implant team for pediatric patients and the team of pediatric speech therapists of our department for their support in realizing this work.
Materials
| Audiointerface | any | Audiointerface with Stereo Line Input is required to Record Acoustic Signal in the Ear Canal for Deriving the Ear Drum Impedance Pattern | |
| Cable Clips | any | Cable Clips for fixation of the Probe Cable at the Head Band | |
| Desktop Computer or Notebook | any | Required for Cochlear Implant Programming Software | |
| Ear Probe | Bio-Logic | Ear Probe for Presenting and Recording Acoustic Signals in the Ear Canal | |
| Head Band | any | Head Band for fixation of the Ear Probe | |
| Maestro Software | Med-El | Programming Software for Med-El Cochlear Implants | |
| MAX Coil | Med-El | Cable connecting Interfacebox and Cochlear Implant via Transcutaneous Inductive Coupling for Telemetry Measurement | |
| MAX Interface Box | Med-El | Interfacebox to access Cochlear Implant during the Fitting Session | |
| MAX Programming Cable | Med-El | Cable connecting Interfacebox and Audioprocessor for Adjusting Electrical Stimulation Levels | |
| Single use Ear Tips | Sanibel Supply | Ear Tips for Ear Probe, Size depending on the Patients Ear | |
| Sonnet 2 Audioprocessor | Med-El | External Part of the Implant System. Has to be worn by the Patient to Perceive Auditory Sensations |
References
- Kosaner, J., Anderson, I., Turan, Z., Deibl, M. The use of ESRT in fitting children with cochlear implants. J. Int Adv Otol. 5 (1), 62-71 (2009).
- Gordon, K. A., Papsin, B. C., Harrison, R. V. Toward a battery of behavioral and objective measures to achieve optimal cochlear implant stimulation levels in children. Ear hear. 25 (5), 447-463 (2004).
- Stephan, K., Welzl-Müller, K., Stiglbrunner, H. Stapedius reflex threshold in cochlear implant patients. Audiology. 27 (4), 227-233 (1988).
- Stephan, K., Welzl-Müller, K. Post-operative stapedius reflex tests with simultaneous loudness scaling in patients supplied with cochlear implants. Audiology. 39 (1), 13-18 (2000).
- Allum, J. H., Greisiger, R., Probst, R. Relationship of intraoperative electrically evoked stapedius reflex thresholds to maximum comfortable loudness levels of children with cochlear implants. Int. J. Audiol. 41 (2), 93-99 (2002).
- Kosaner, J. Generating speech processor programmes for children using ESRT measurements. CI International. 11, 20-24 (2010).
- Walkowiak, A., et al. Evoked stapedius reflex and compound action potential thresholds versus most comfortable loudness level: assessment of their relation for charge-based fitting strategies in implant users. ORL J Otorhinolaryngol Relat Spec. 73 (4), 189-195 (2011).
- Stephan, K., Welzl-Müller, K. Effect of stimulus duration on stapedius reflex threshold in electrical stimulation via cochlear implant. Audiology. 33 (3), 143-151 (1994).
- Stephan, K. A fast response impedance meter for acoustic reflex measurements. IEEE Trans. Biomed. Eng. 41, 391-393 (1994).
- Litovsky, R. Y., Gordon, K. Bilateral cochlear implants in children: Effects of auditory experience and deprivation on auditory perception. Hear. Res. 338, 76-87 (2016).
- Franke-Trieger, A., Mattheus, W., Seebacher, J., Zahnert, T., Neudert, M. Stapedius reflex evoked in free sound field in cochlear implant users compared to normal-hearing listeners. Int. J. Audiol. 60 (9), 695-703 (2021).
- Franke-Trieger, A., et al. Stapedius reflex thresholds obtained in a free sound field as an indicator for over- and understimulation in cochlear implant listeners. Int. J. Audiol. , 1-8 (2023).
- Crawford, M. W., et al. Dose-dependent suppression of the electrically elicited stapedius reflex by general anesthetics in children undergoing cochlear implant surgery. Anesth Analg. 108 (5), 1480-1487 (2009).

.
